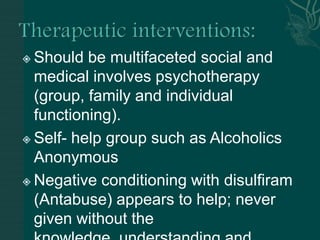
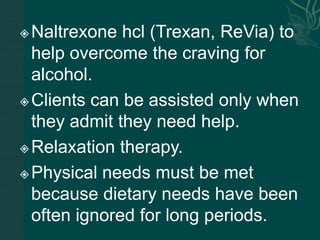
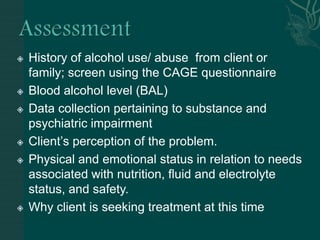
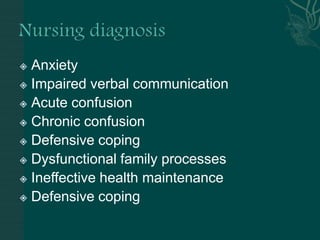
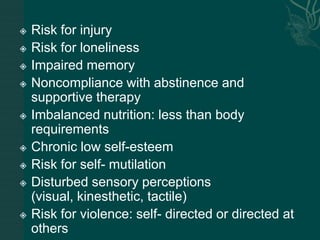
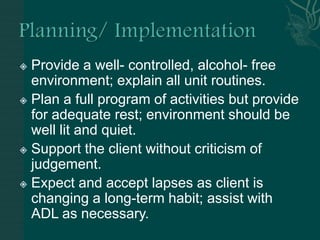
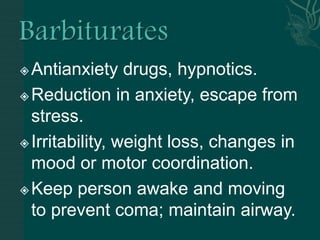
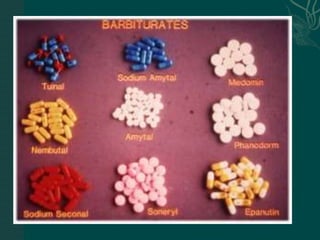
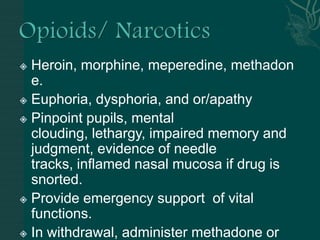
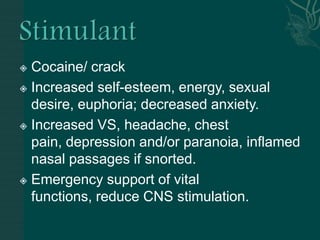
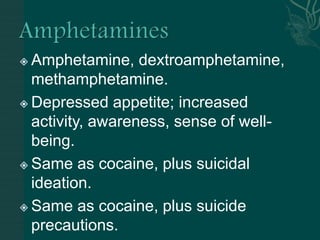
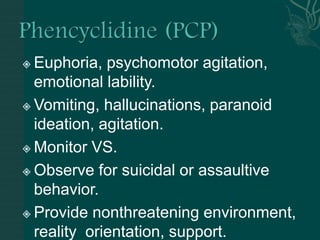
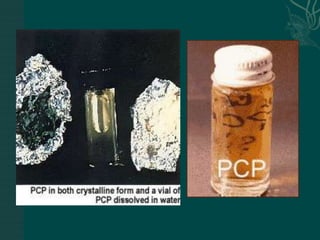
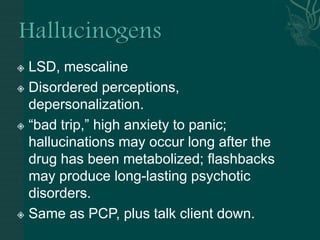
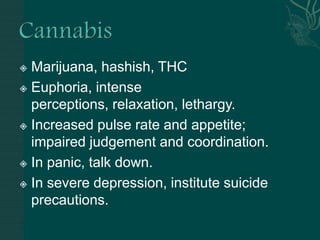
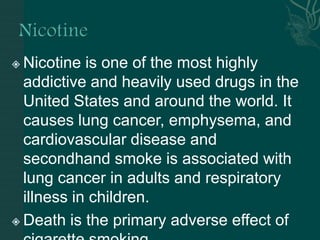
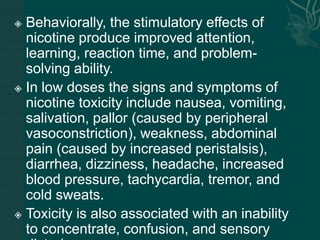
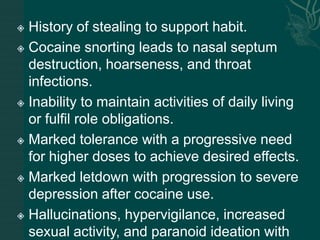
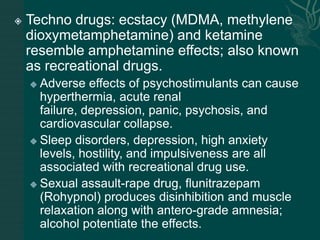
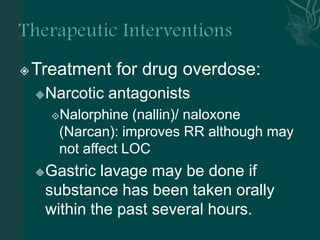
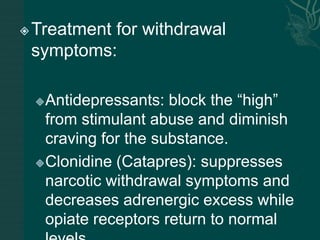
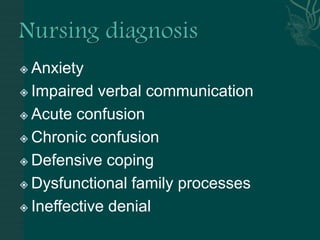
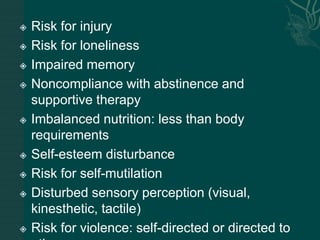
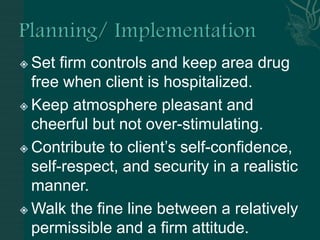
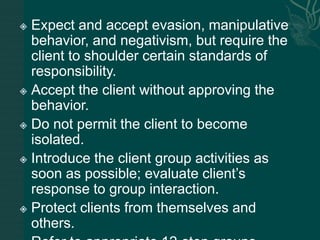
The document discusses substance abuse and addiction. It defines terms like substance, substance abuse, intoxication, withdrawal, tolerance, dependence, and polysubstance abuse. It describes signs and symptoms of use and withdrawal from various substances like alcohol, opioids, cocaine, amphetamines, hallucinogens, marijuana, and nicotine. It discusses treatment approaches including managing overdose, withdrawal symptoms, and long term programs. Nursing considerations are outlined like ensuring a safe environment, supporting the client, and managing risks.