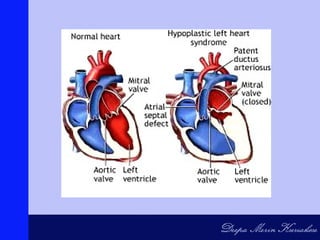
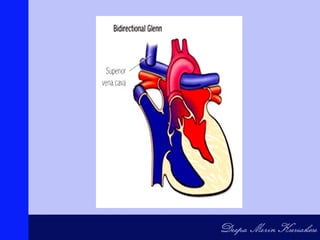
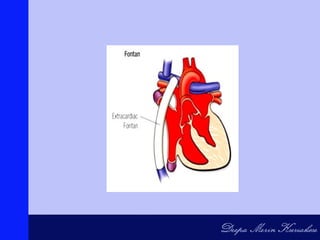
Hypoplastic Left Heart Syndrome (HLHS) occurs when parts of the left side of the heart do not develop completely, making the left ventricle nonfunctional and unable to supply blood to the systemic circulation. It is present at birth and requires ductal patency for systemic blood flow. The condition causes the right side of the heart to maintain circulation for both the lungs and body. Without intervention after ductal closure, shock and death will rapidly occur due to poor organ perfusion. The standard treatment is a staged surgical approach involving three procedures over several years to reconstruct the heart and establish adequate circulation.