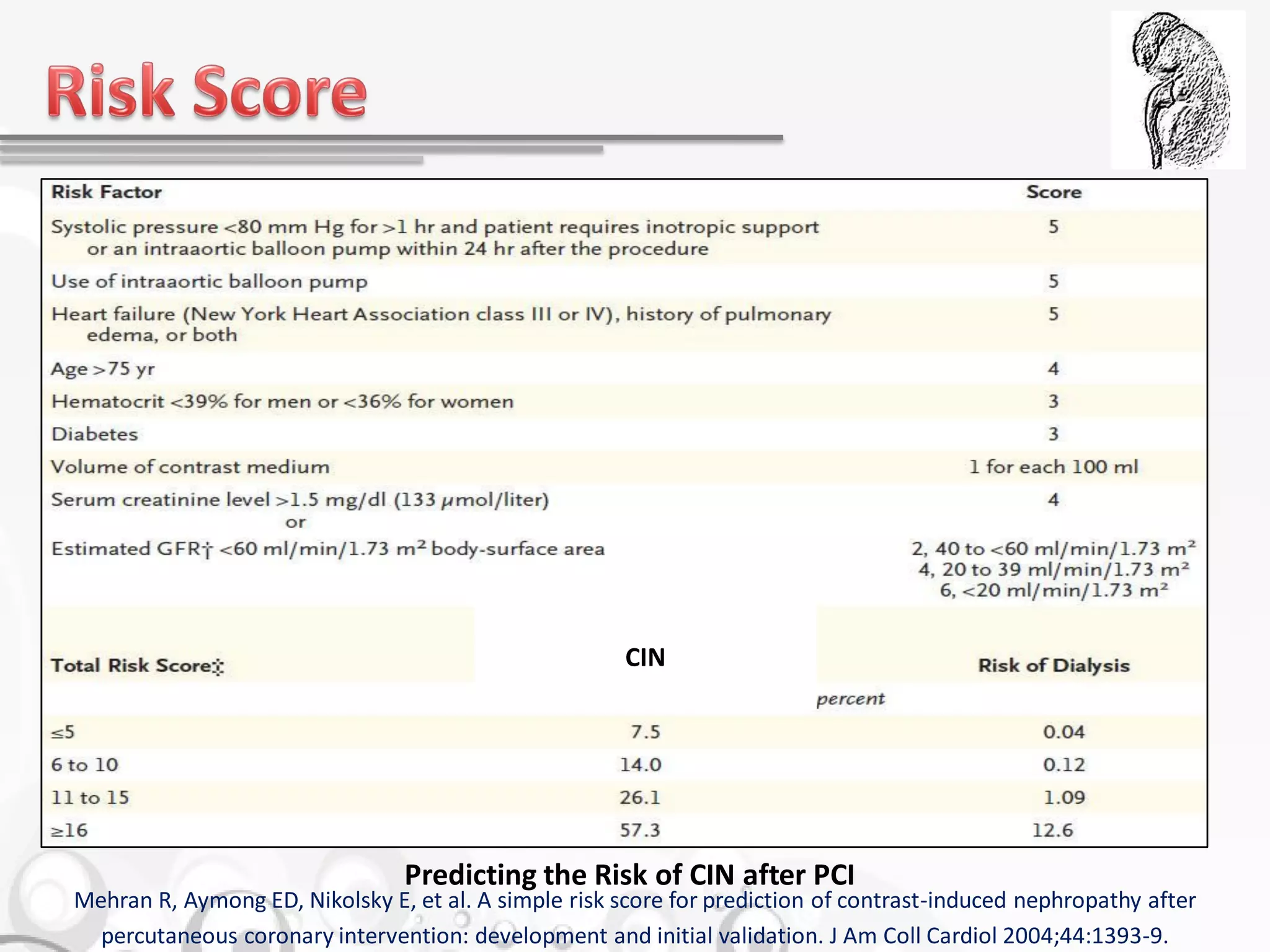
The document discusses contrast-induced nephropathy (CIN), a reversible form of acute kidney injury that can occur after the administration of radiocontrast media. It highlights risk factors, the significance of hydration and preventive strategies, and various treatments and medications to mitigate CIN, including acetylcysteine and hydration protocols. The document emphasizes that prevention is crucial, and measures should be taken to minimize the risk, particularly in high-risk patients.