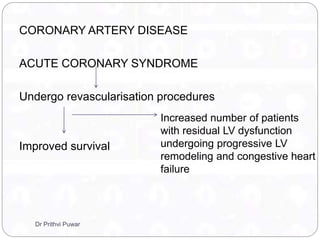
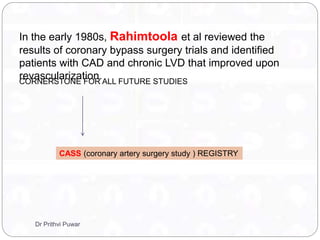
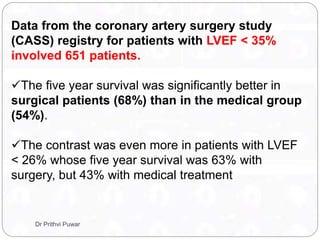
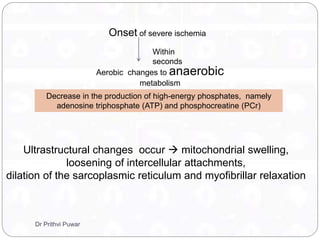
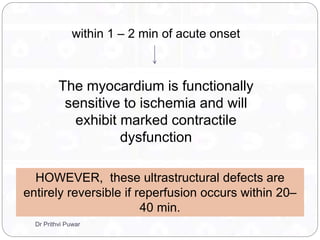
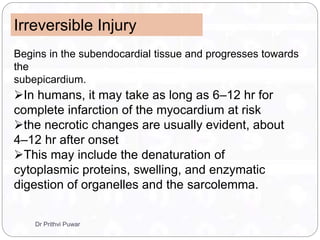
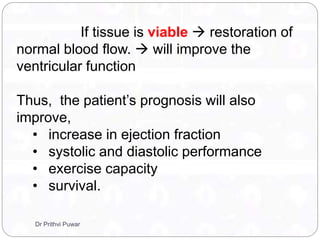
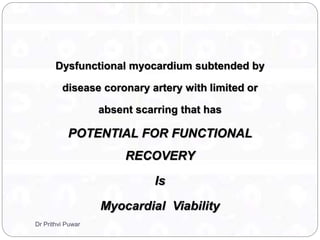
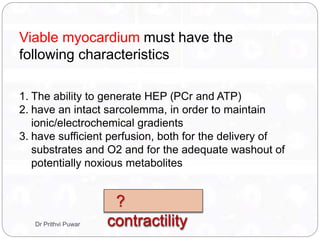
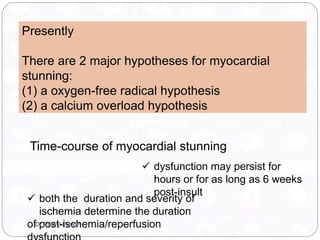
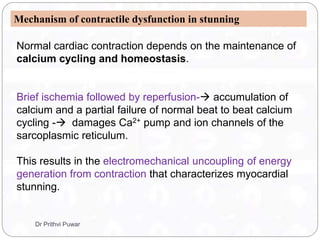
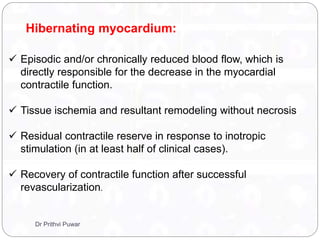
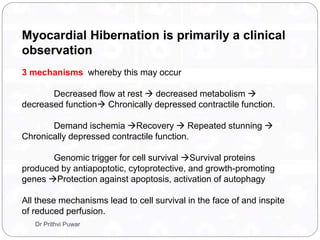
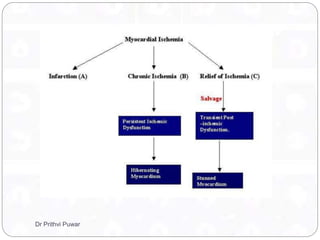
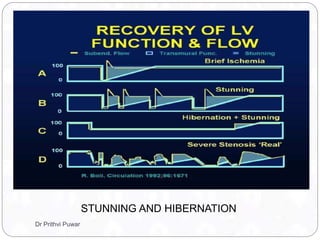
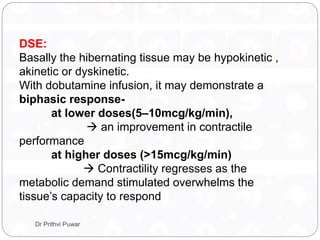
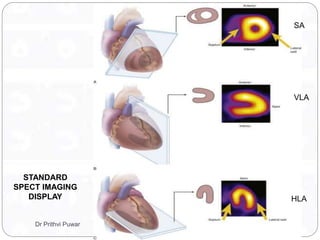
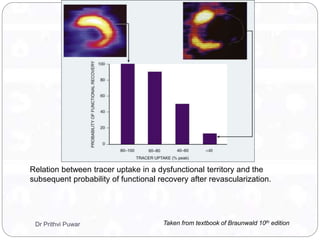
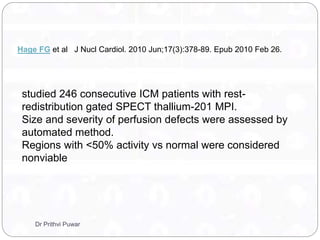
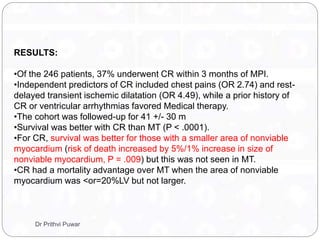
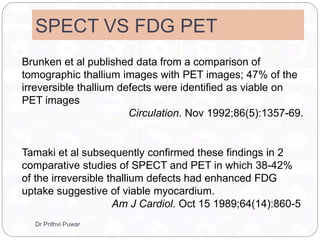
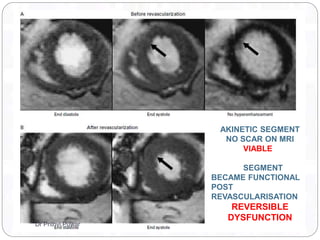
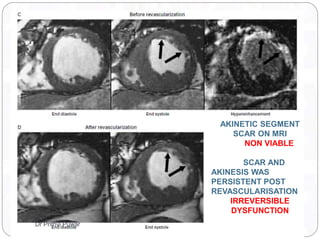
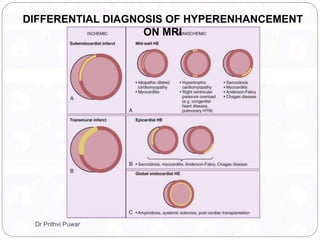
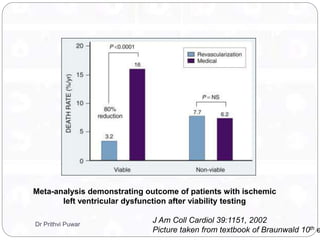
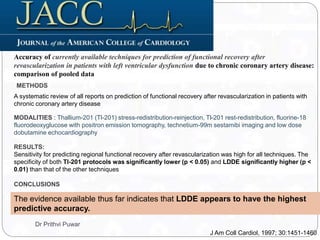
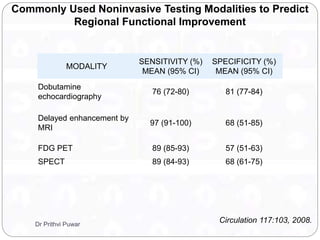
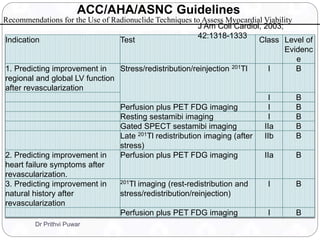
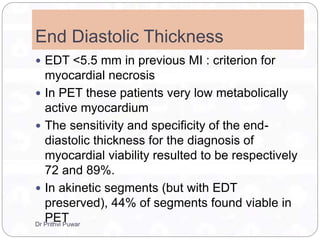
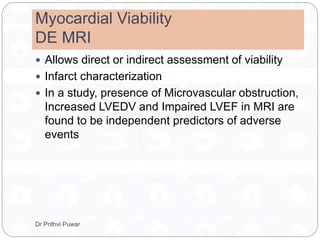
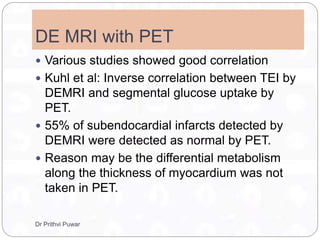
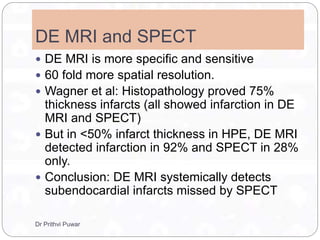
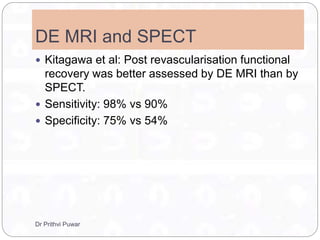
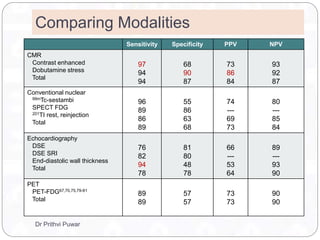
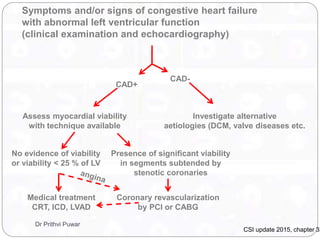
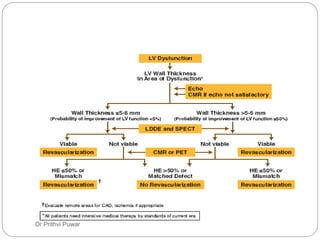
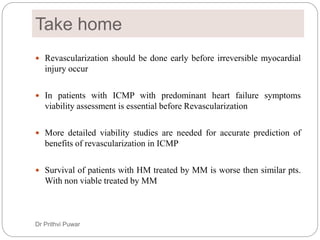
Dr. Prithvi Puwar explores myocardial viability in patients with coronary artery disease and the impact of revascularization procedures on improving survival and ventricular function. The document discusses key concepts such as myocardial stunning and hibernation, delineating the factors underlying contractile dysfunction and the importance of assessing myocardial viability through various non-invasive imaging modalities. Techniques like echocardiography, SPECT, PET, and cardiac MRI are evaluated for their roles in identifying viable myocardium and predicting patient outcomes following ischemic events.