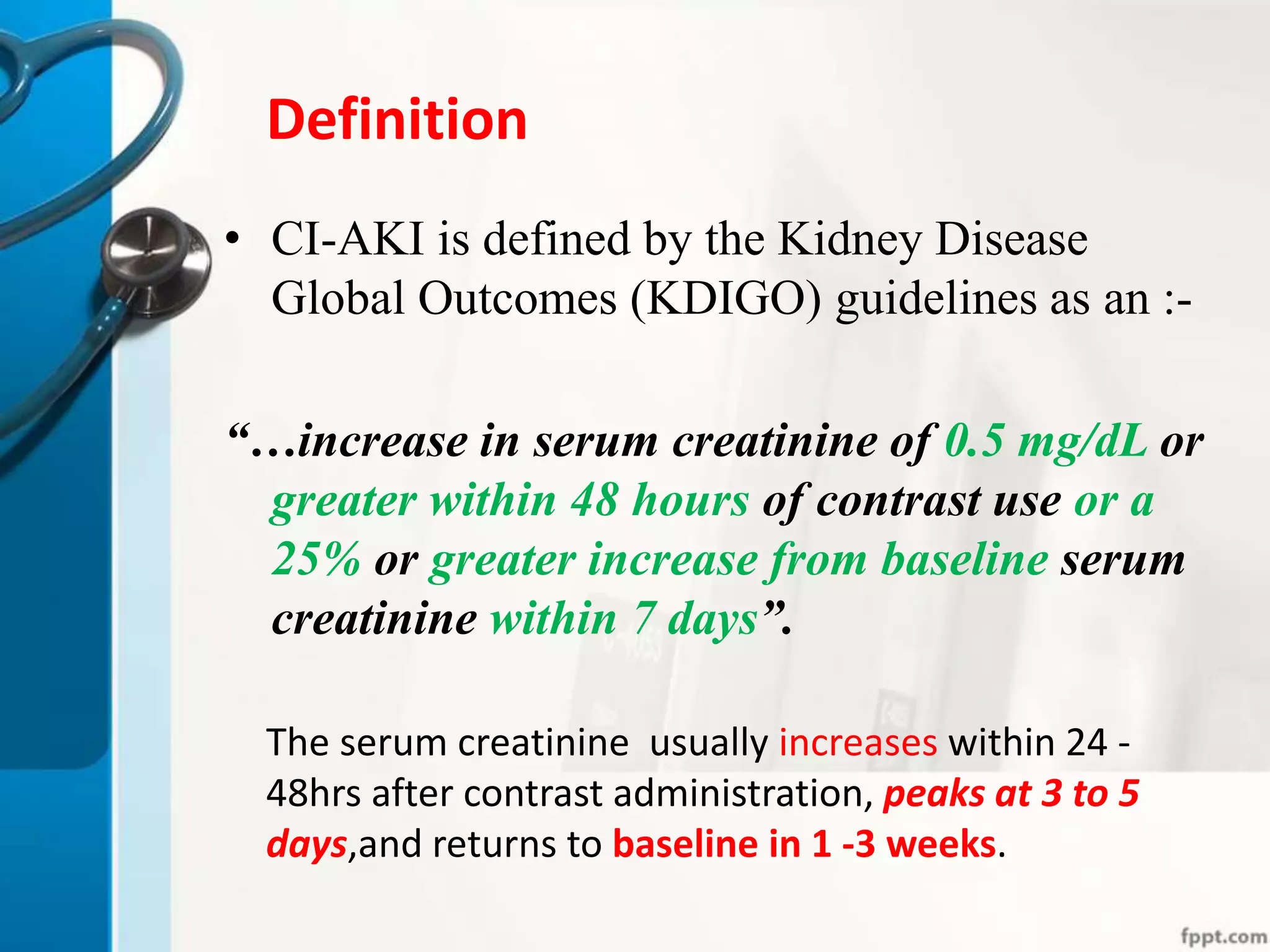
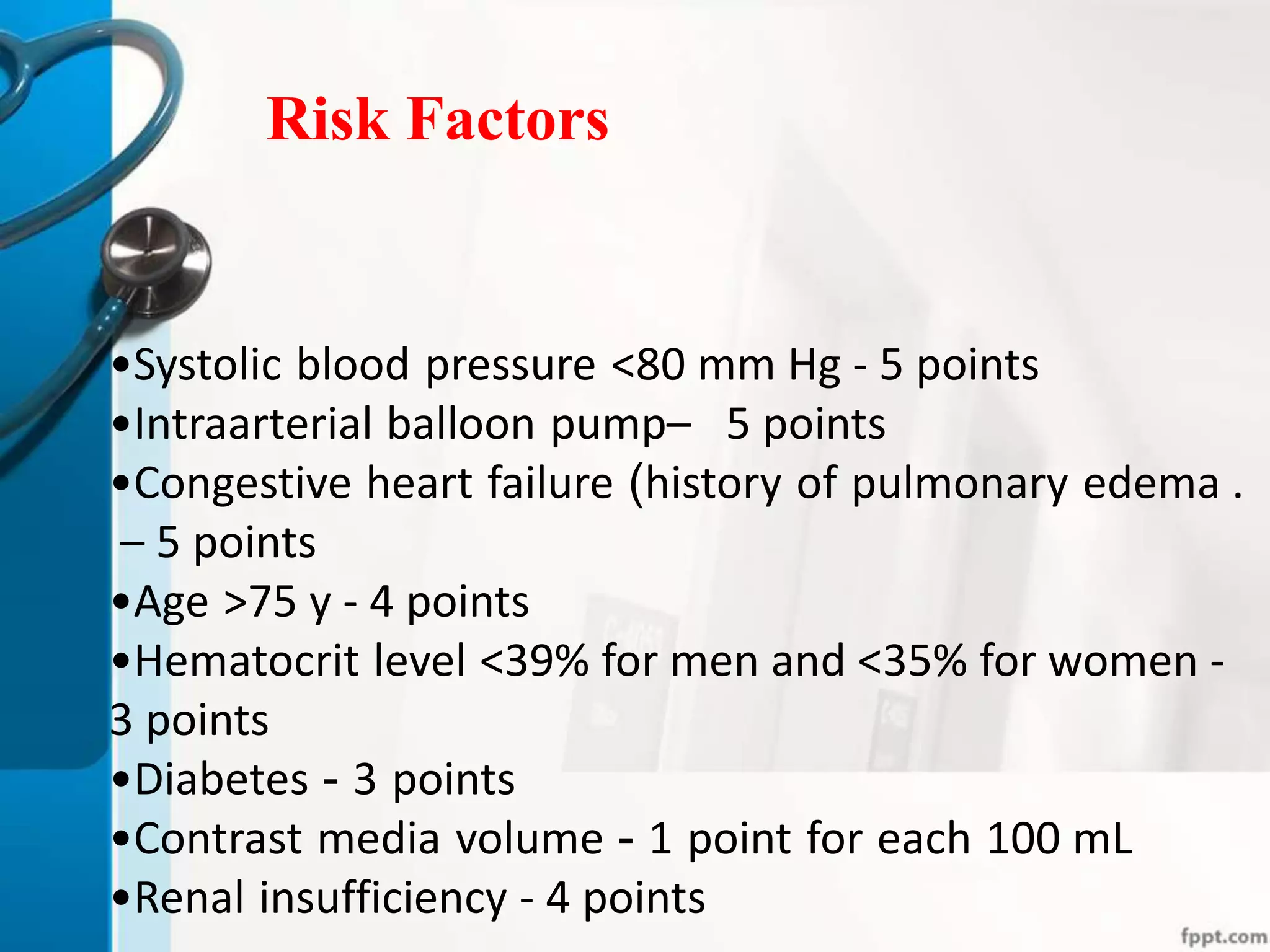
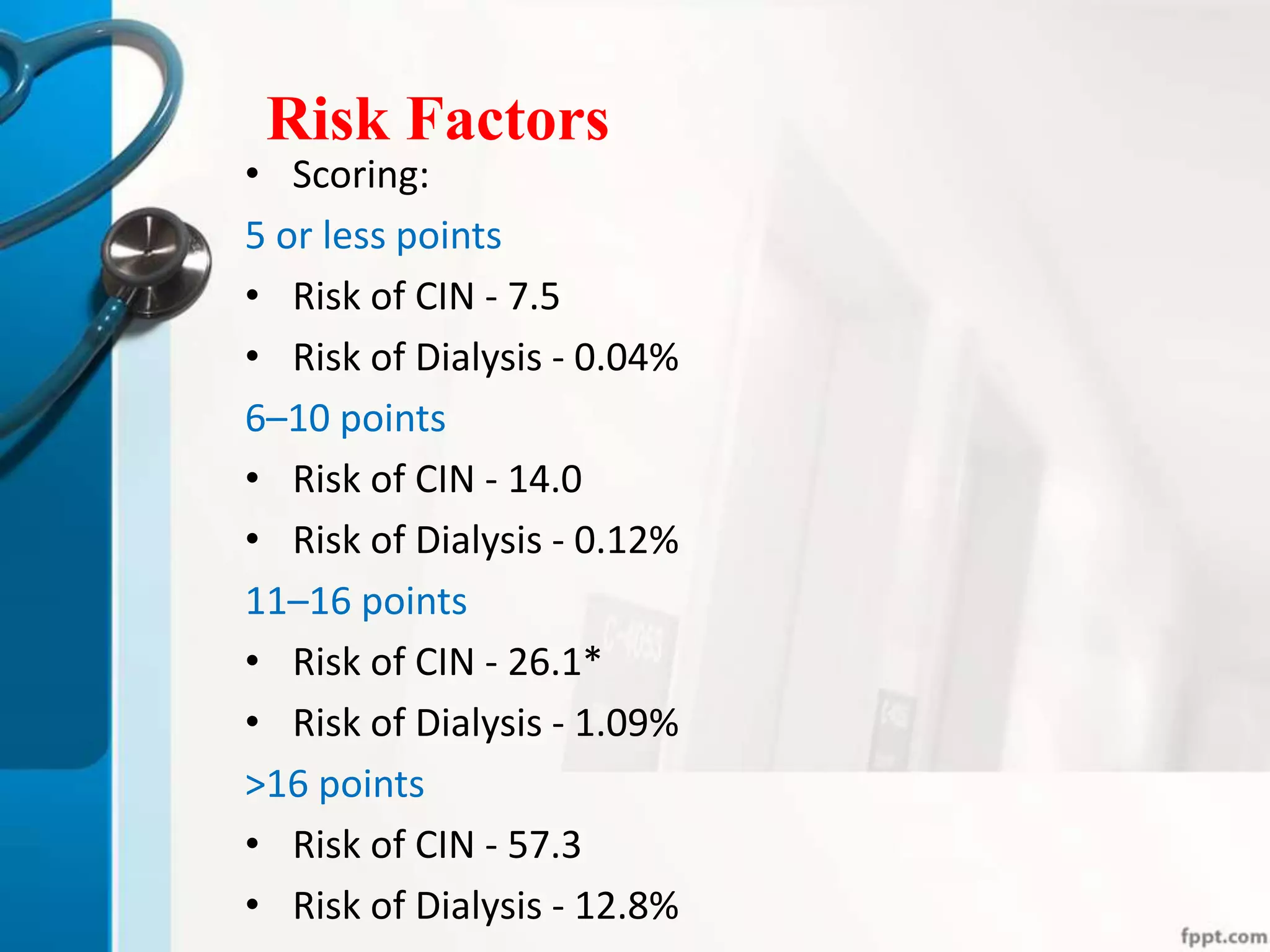
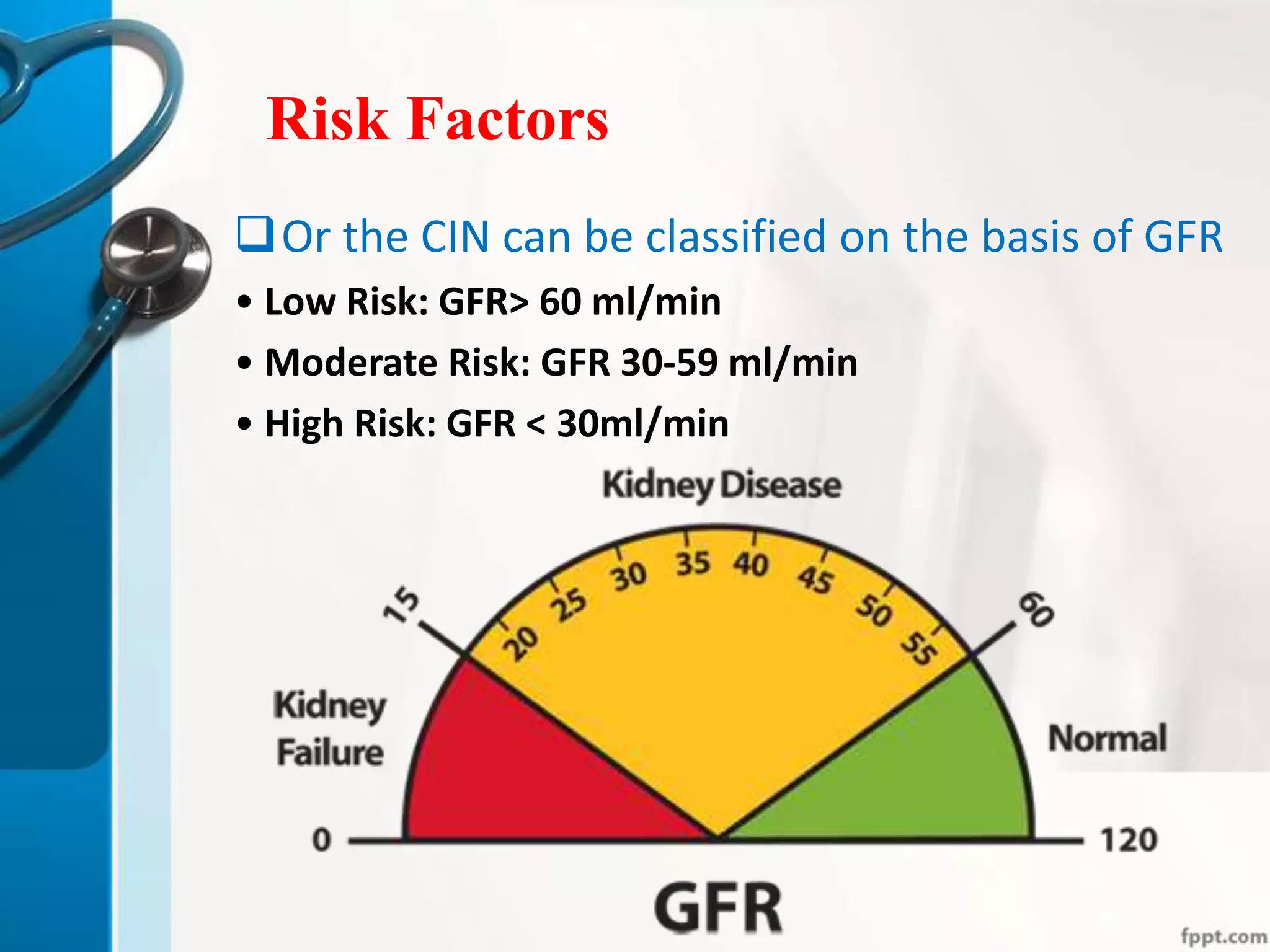
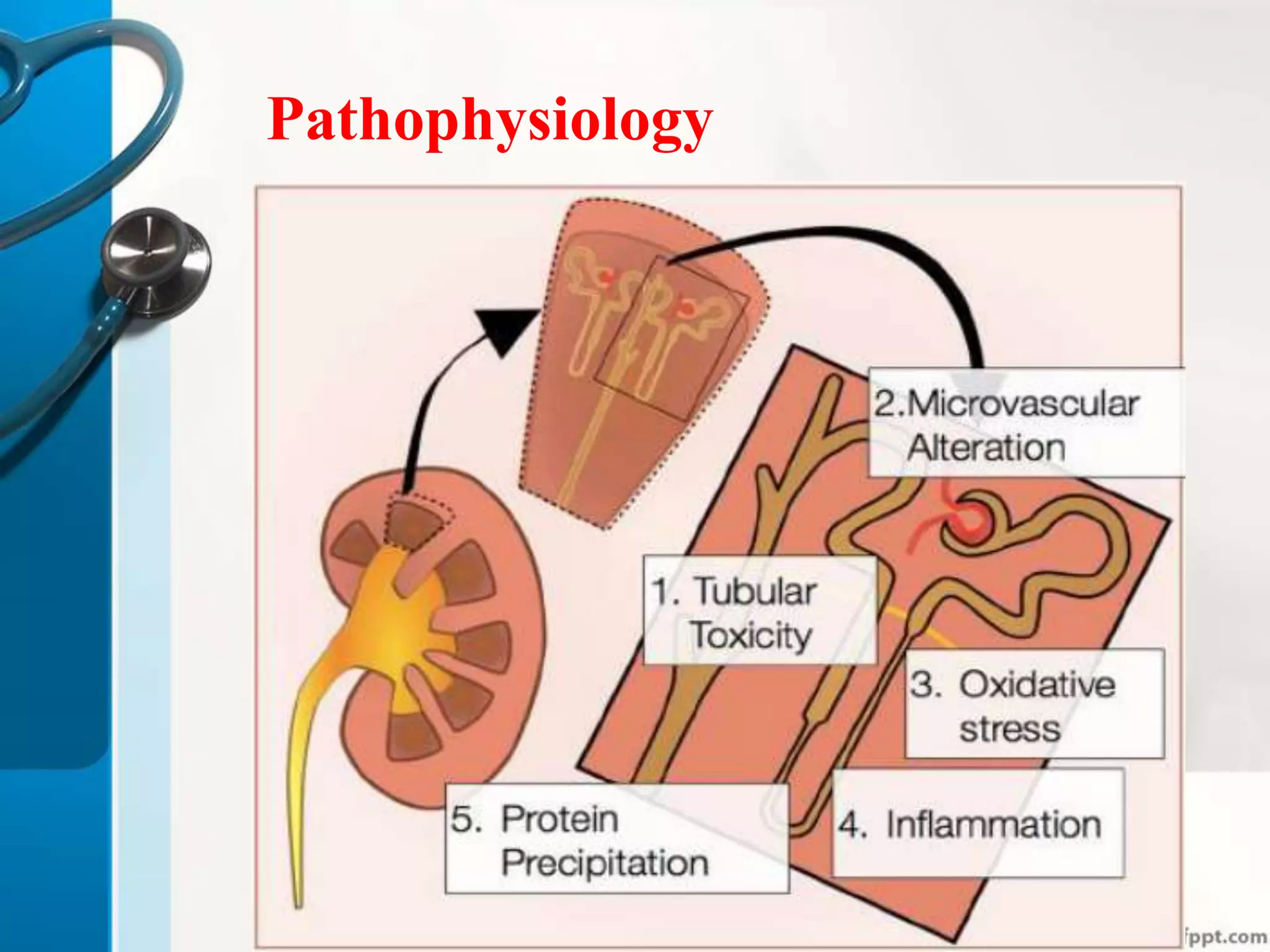
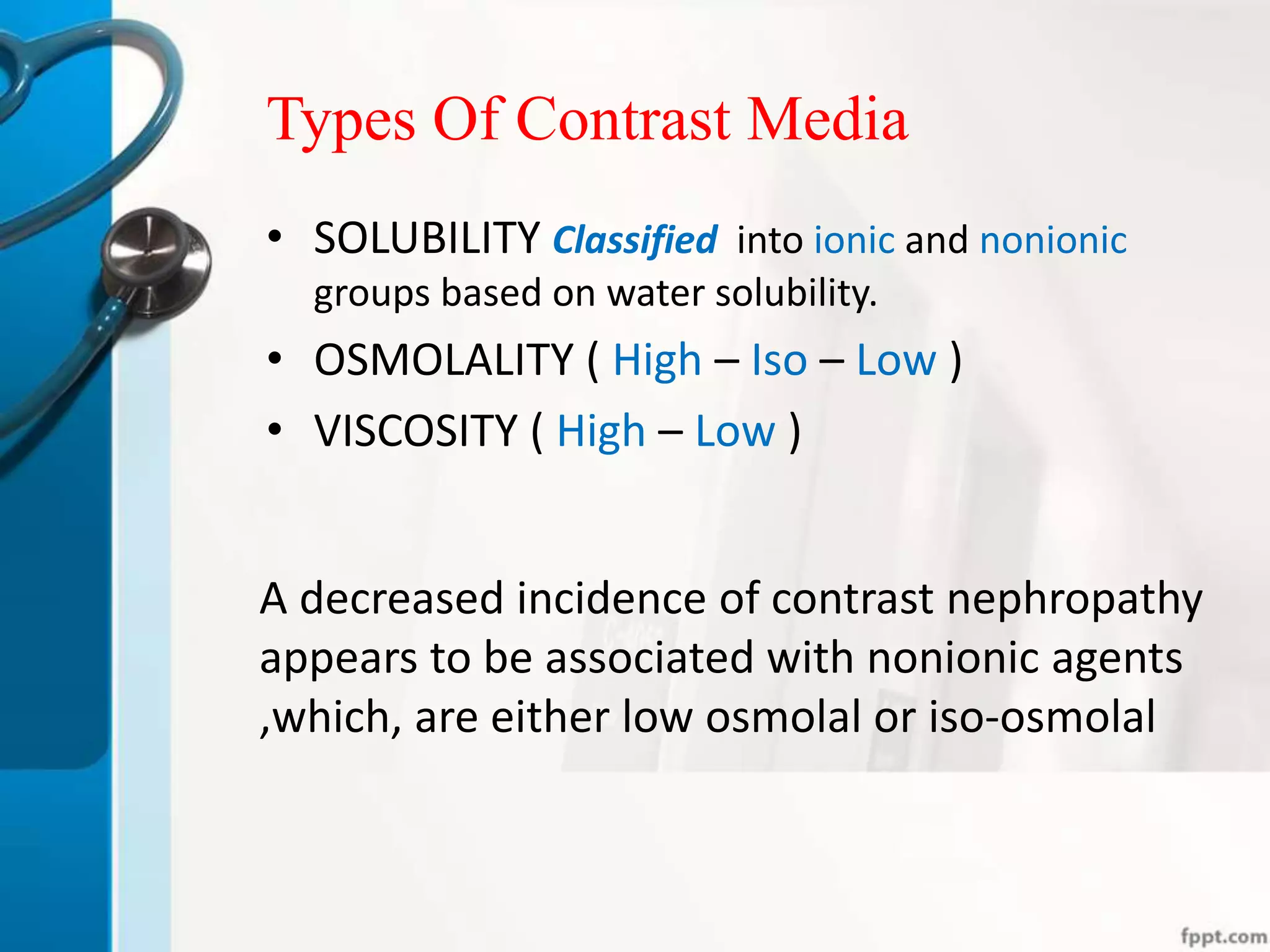
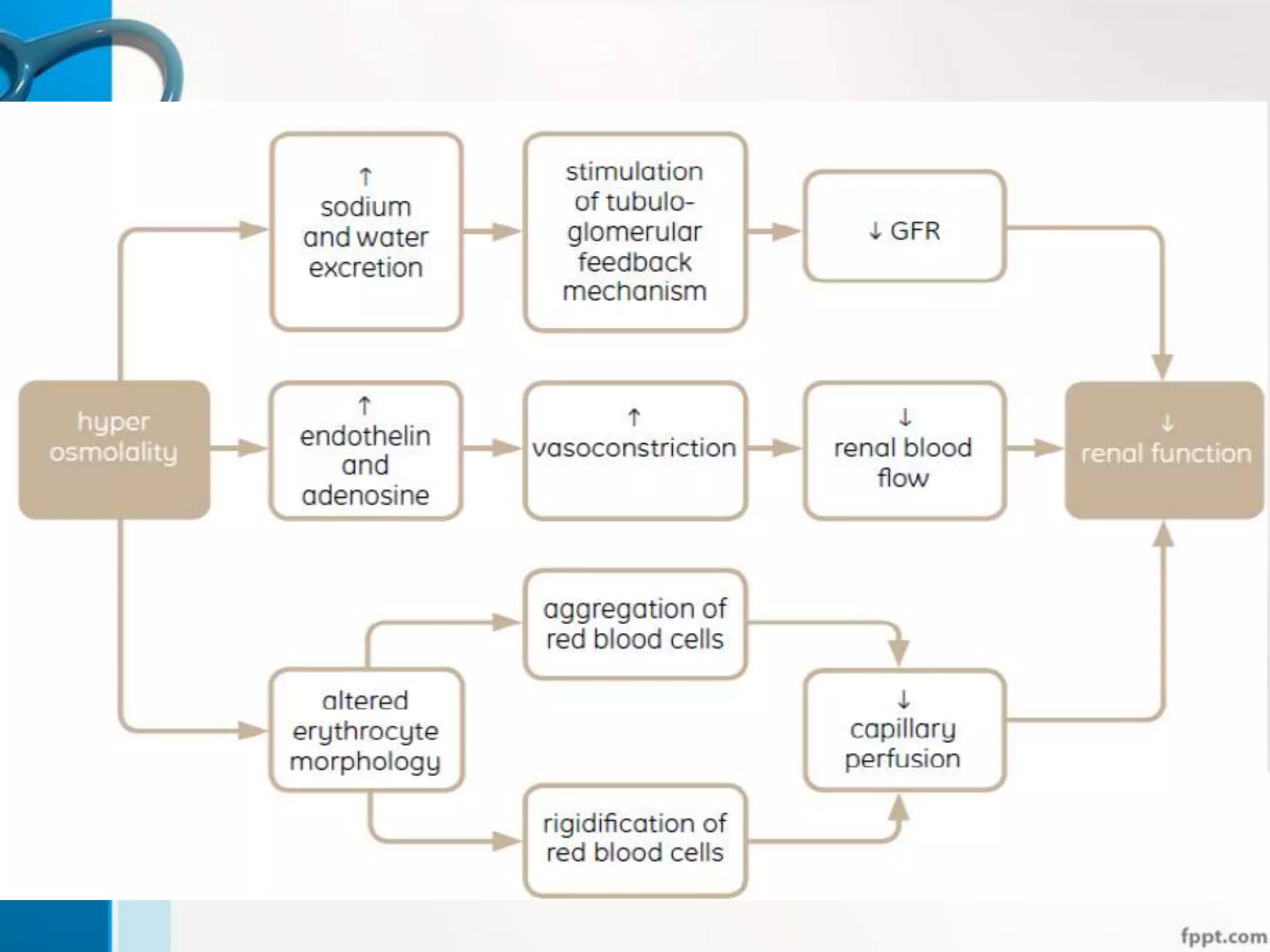
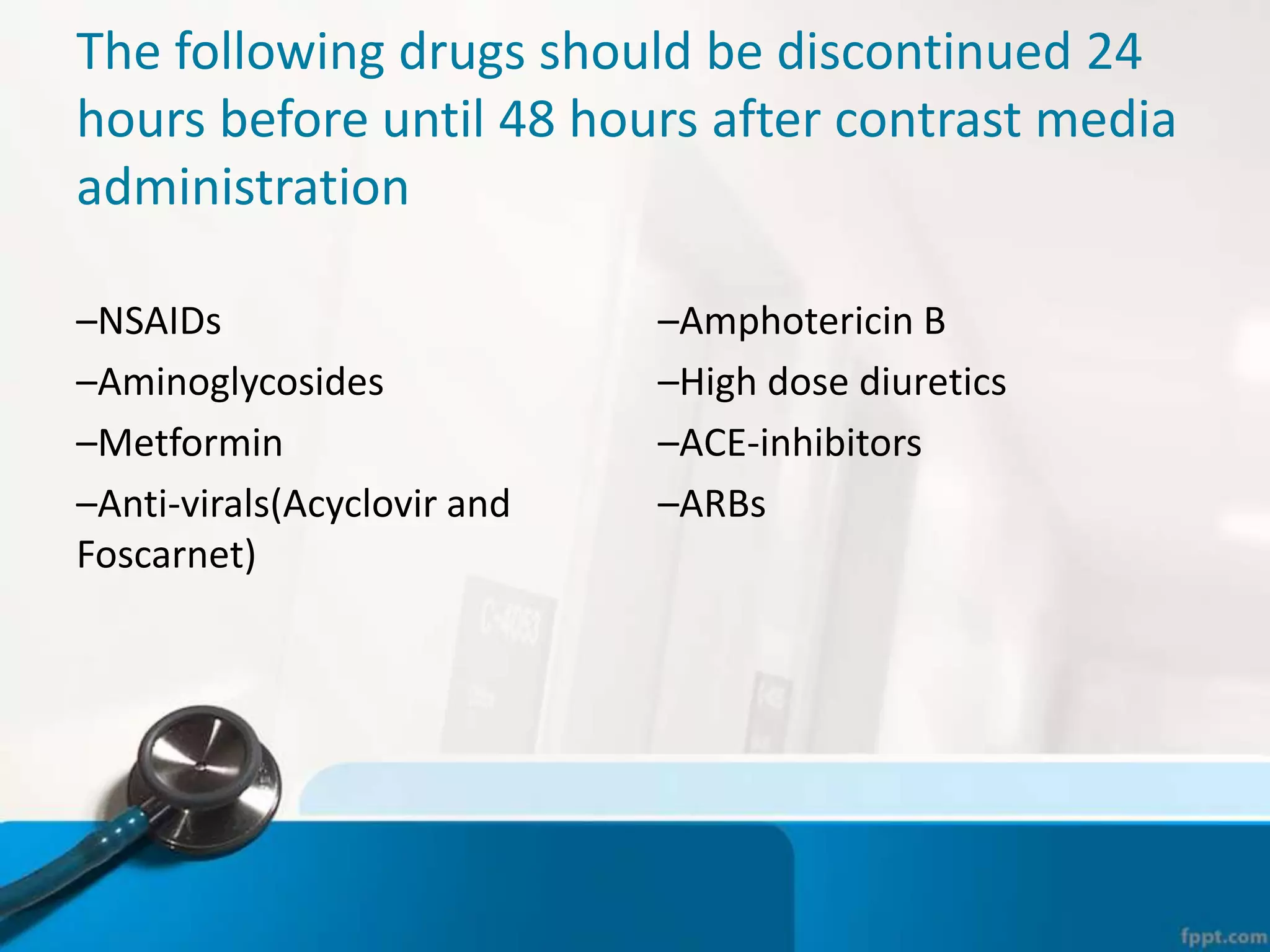
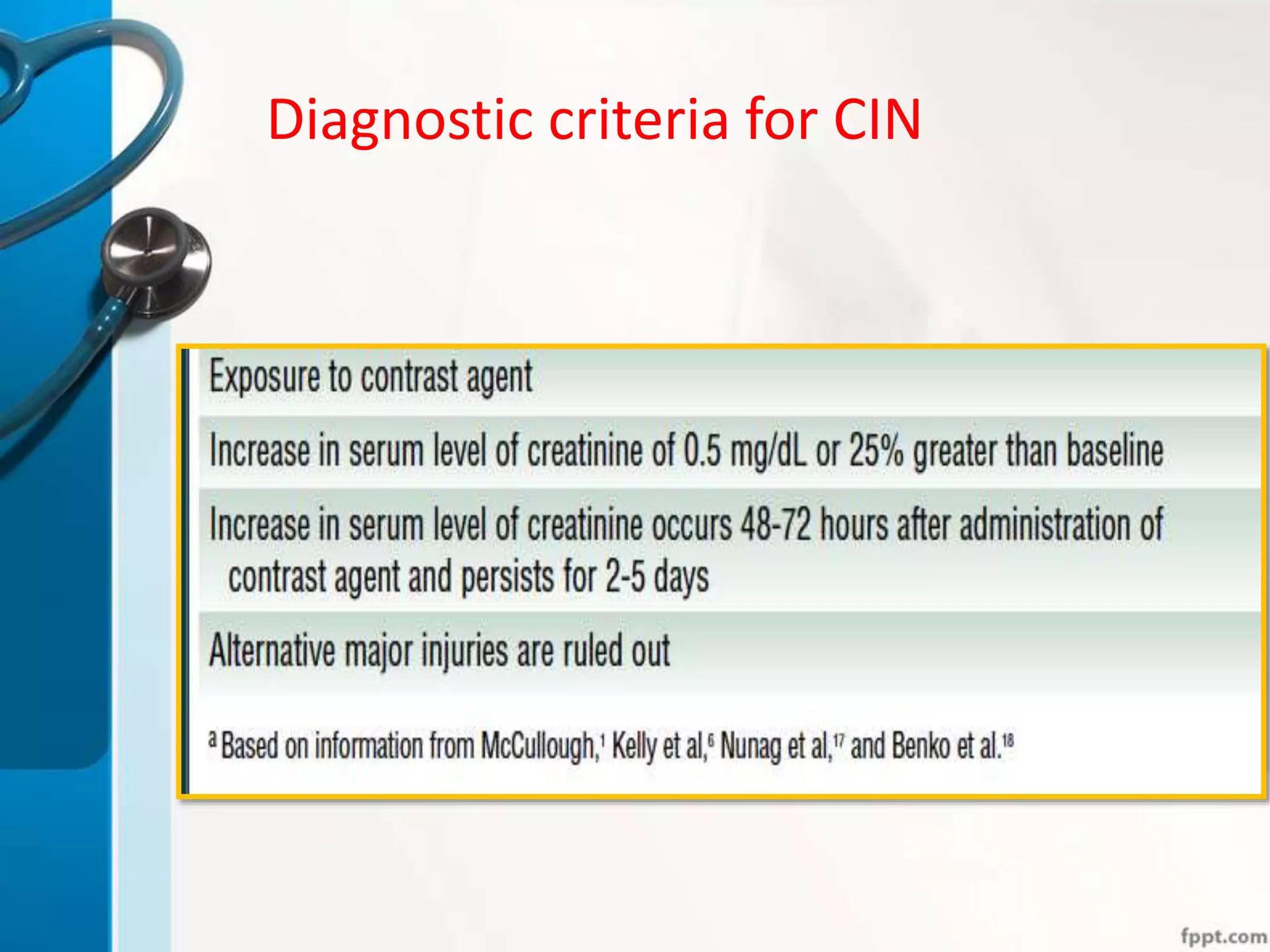
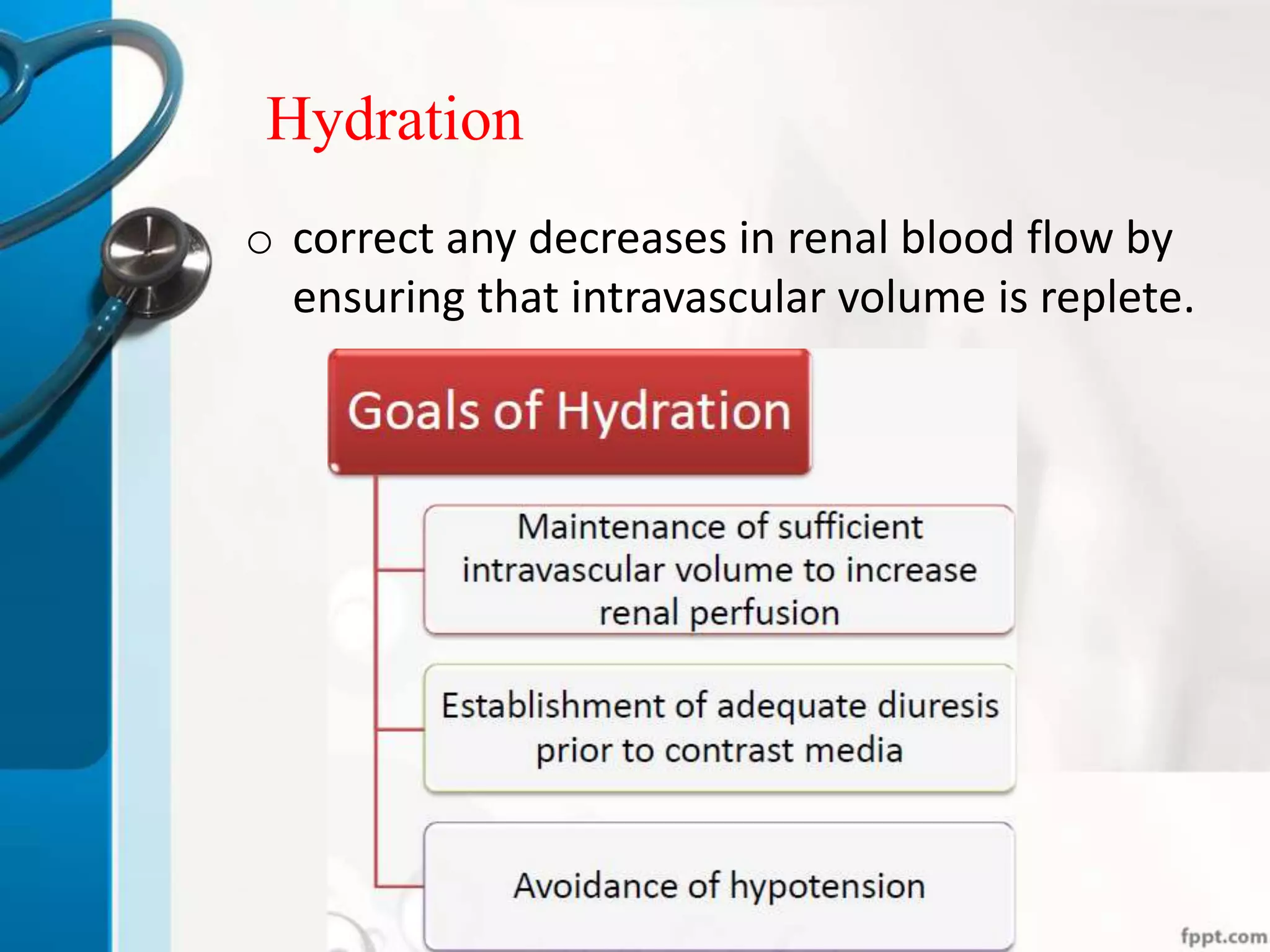
Contrast-induced nephropathy (CIN) is a significant cause of acute kidney injury, particularly in hospitalized patients undergoing endovascular procedures. Defined by specific criteria related to serum creatinine levels, CIN may be influenced by various risk factors, including baseline renal function and certain medications. Management focuses on prevention through hydration and appropriate contrast media usage, with the effectiveness of various pharmacological agents still under investigation.