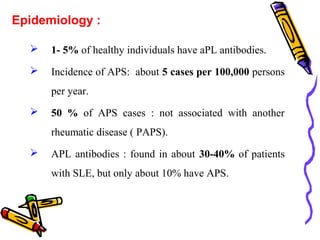
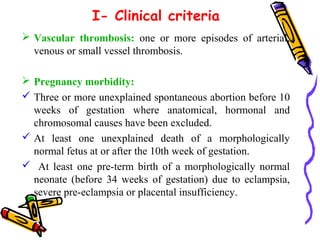
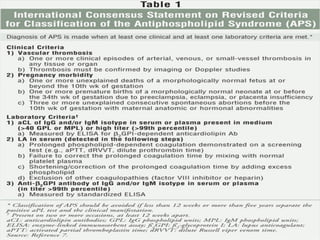
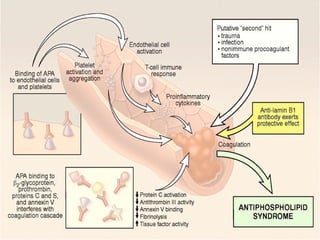
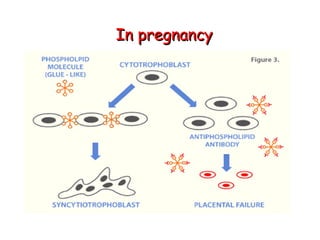
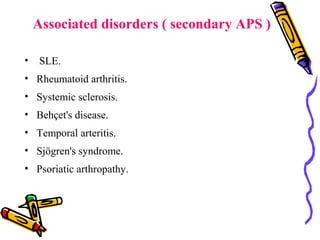
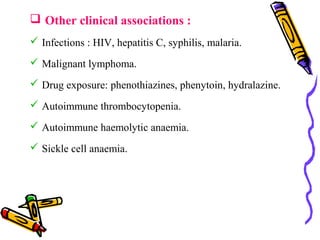
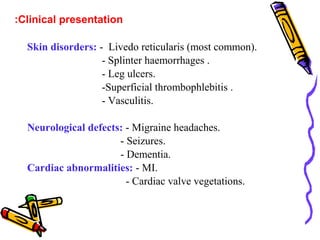
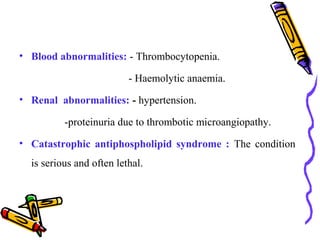
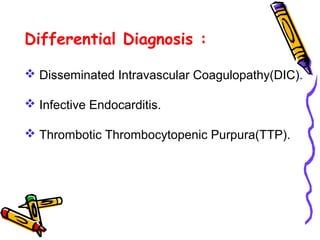
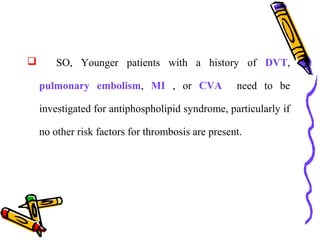
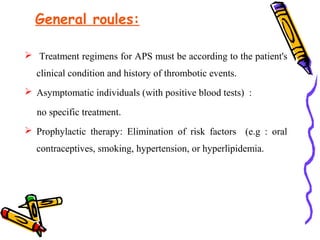
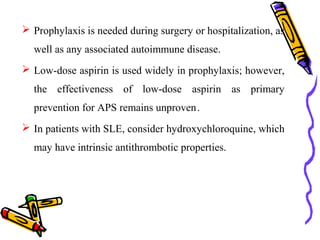
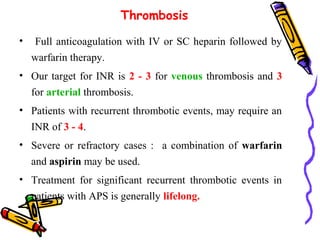
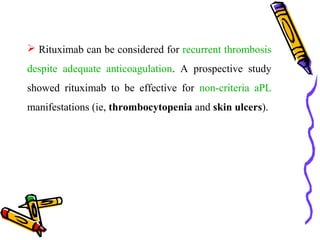
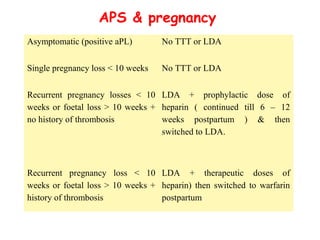
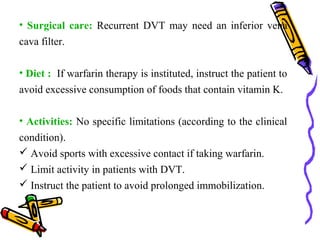
Antiphospholipid syndrome (APS) is an autoimmune disorder characterized by blood clots in arteries and veins, pregnancy complications, and the presence of antiphospholipid antibodies. The syndrome can occur alone or in association with other autoimmune diseases like lupus. Treatment involves long-term anticoagulation with blood thinners and aspirin to prevent new clots from forming. Management of pregnancy in APS patients depends on their history and involves low-dose aspirin with or without low or high dose blood thinners.