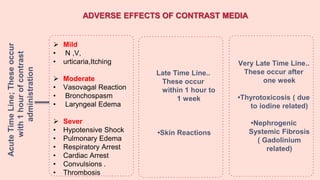
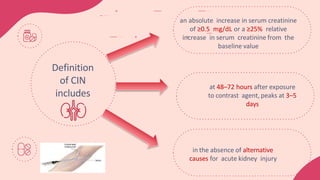
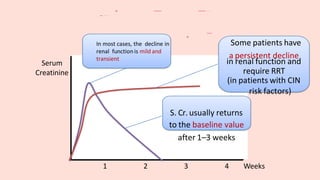
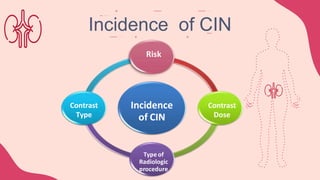
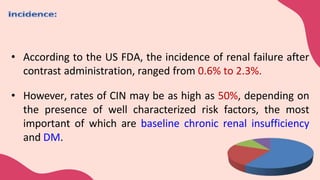
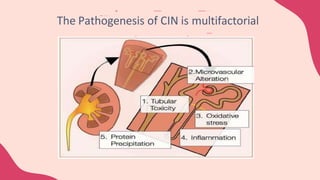
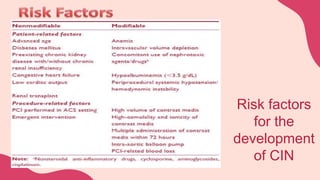
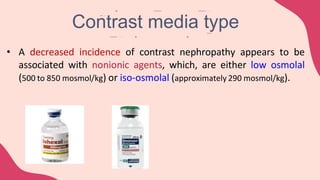
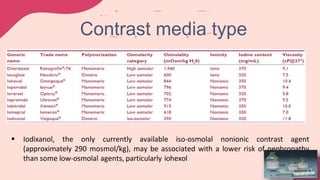
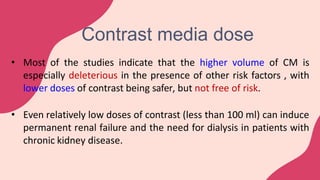
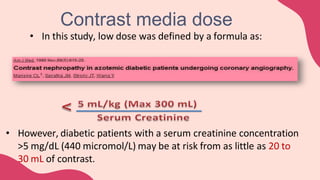
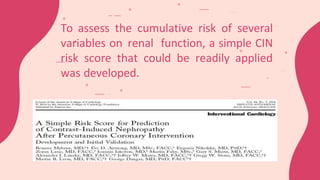
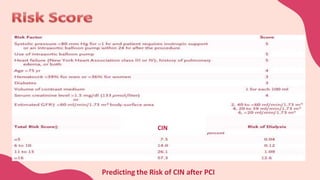
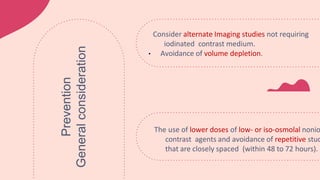
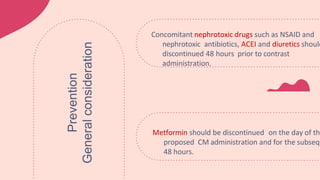
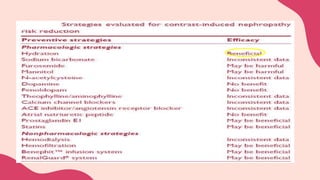
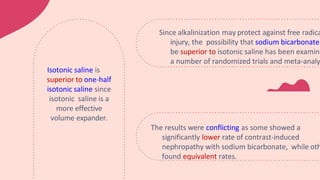
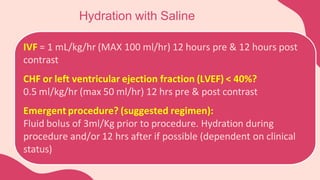
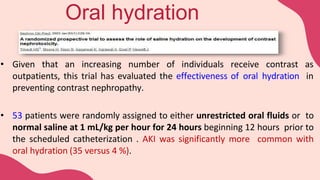
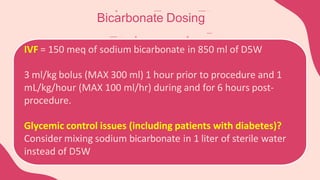
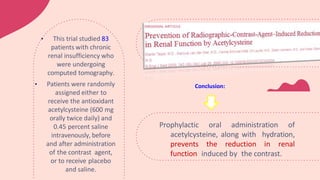
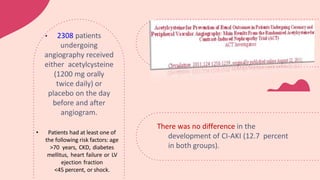
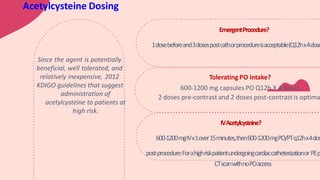
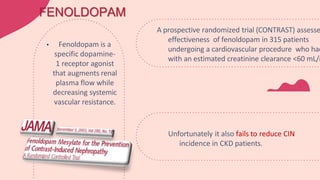
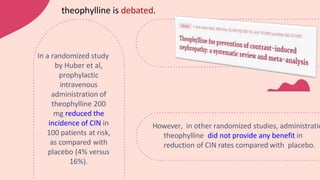
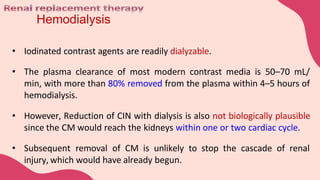
This document provides information on contrast induced nephropathy (CIN), including its definition, pathogenesis, risk factors, incidence, prevention, and management. CIN is a form of acute kidney injury caused by radiocontrast media administration that results in an increase in serum creatinine levels within 3 days. Prevention focuses on hydration, using low- or iso-osmolar contrast agents, avoiding repetitive procedures, and discontinuing nephrotoxic drugs. Treatment is supportive as CIN is generally reversible with hydration and supportive care.