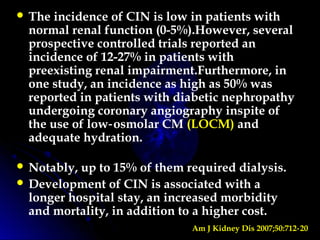
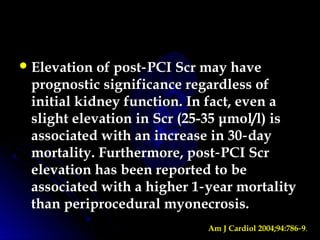
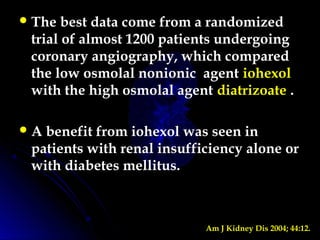
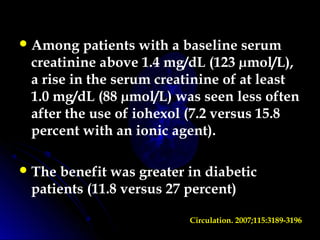
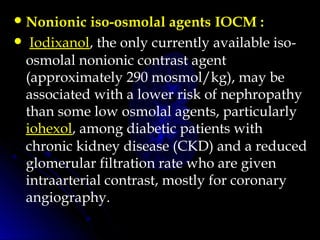
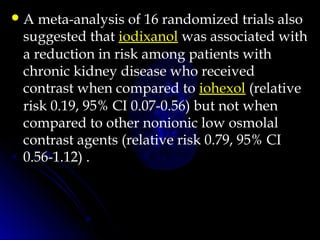
Contrast-induced nephropathy (CIN) is a common cause of hospital-acquired acute kidney injury. The risk of developing CIN is highest in patients with preexisting chronic kidney disease, diabetes, or those receiving a high volume of contrast agent. Nonionic, low-osmolar contrast agents have been shown to reduce the risk of CIN compared to ionic, high-osmolar agents. Preventive strategies focus on minimizing contrast volume, adequate hydration, and avoiding nephrotoxic medications.
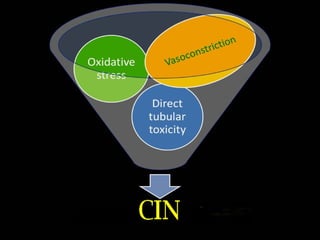
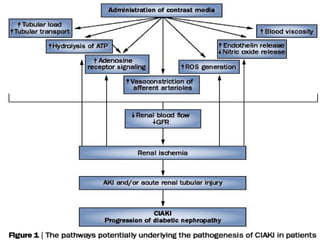
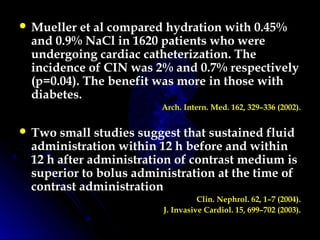
![•Oxidative stress:
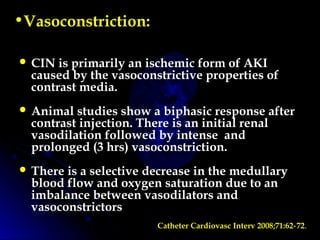
The intense vasoconstriction and loss of
autoregulatory capacity can contribute to
additional renal injury through the release of
reactive oxygen species (eg, superoxide [OH].).
Damage is due to overwhelming of the anti-
oxidant factors by the excess generation of
ROS.
Underlying diseases like CKD and Diabetes
already have high ROS and thus predisposes
for CIN.
Benefit of anti-oxidants gives an indirect clue.](https://image.slidesharecdn.com/cin-160602182032/85/CIN-13-320.jpg)
![ There appears to be little or no advantage in
the prevention of contrast nephropathy when
compared to ionic hyperosmolal agents in
patients with normal renal function a group
that is at low risk.
In studies of patients with moderate renal
insufficiency (serum creatinine concentration
between 1.4 and 2.4 mg/dL [123 to 211 µmol/L]),
some nonionic, low osmolality agents
compared to hyperosmolal agents have been
associated with a reduced incidence of a mild
to moderate decline in renal function .](https://image.slidesharecdn.com/cin-160602182032/85/CIN-27-320.jpg)
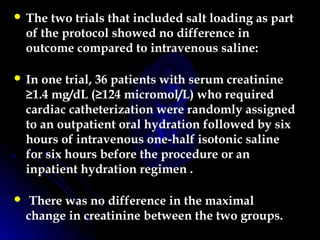
![ The second trial compared salt loading with
tablets (1 g/10 kg per day in two or three doses
for two days before contrast) and saline
hydration (15 mL/kg for six hours prior to
contrast) in 153 patients with CKD (mean
serum creatinine 2.2 mg/dL [200 micromol/L]) .
There was no difference in the proportion of
patients with an increase in serum creatinine of
≥0.5 mg/dL (44 micromol/L) between the two
groups.
Thus, the safety and efficacy of oral hydration
or salt loading for the prevention of contrast
nephropathy remains uncertain.
Nephrol Dial Transplant 2006; 21:2120.](https://image.slidesharecdn.com/cin-160602182032/85/CIN-49-320.jpg)