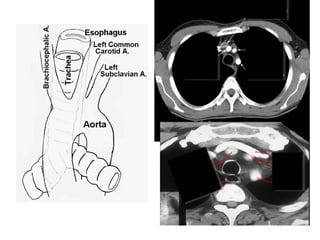
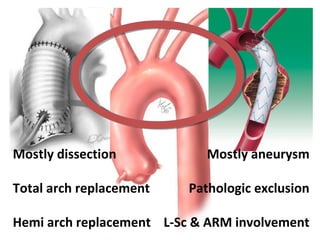
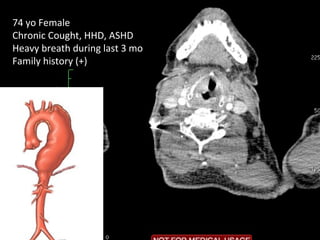
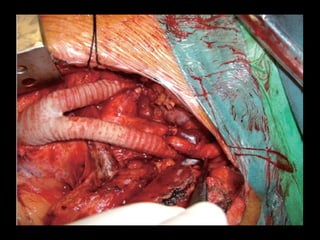
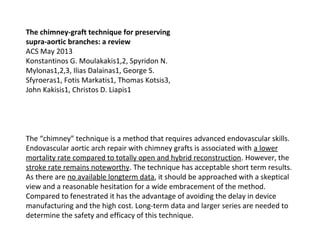
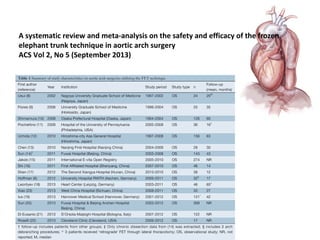
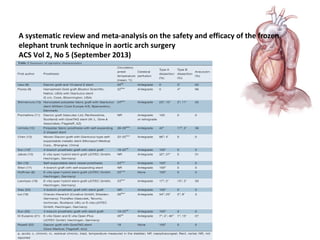
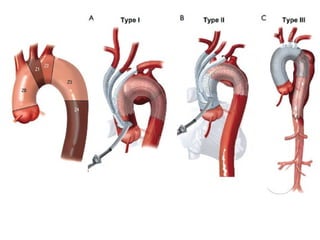
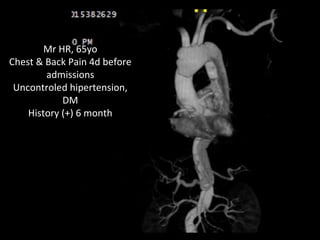
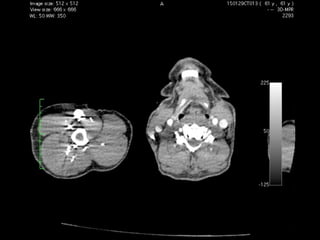
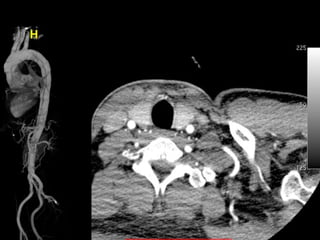
This document summarizes Dicky Aligheri's experience with hybrid procedures for aortic arch involvement between 2013-2014 at the National Cardiac & Vascular Centre Harapan Kita in Jakarta. It describes several case studies of patients who received treatments like total arch replacement, hemi arch replacement, and the frozen elephant trunk procedure. It also reviews literature on debates around the best surgical strategies for aortic arch pathology and the safety and efficacy of hybrid techniques compared to open surgery.







![Interact Cardiovasc Thorac Surg.
2015 Jan;20(1):120-6. doi:
10.1093/icvts/ivu323. Epub 2014 Oct
3.
Is extended arch replacement
justified for acute type A aortic
dissection?
In [patients undergoing surgery, for acute type A aortic dissection] does
[aggressive initial treatment with total arch repair] result in [reduced mortality
and improved closure of the distal false lumen]?
Medline 1950 to December 2013
We conclude that a more extensive surgical strategy can be justified when it is
based on circumstances, on the individual patient's clinical condition, and on
the anatomical and pathological features of the dissection](https://image.slidesharecdn.com/archfinalharkit2015-150306002458-conversion-gate01/85/Arch-final-harkit2015-__-14-320.jpg)