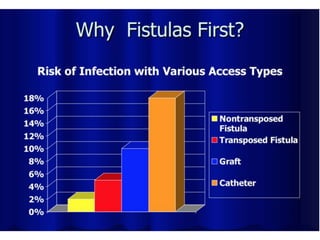
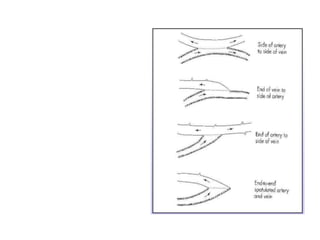
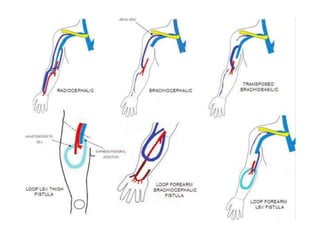
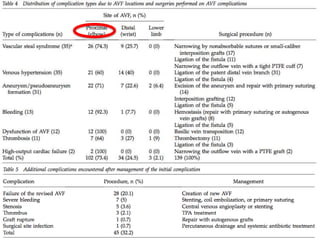
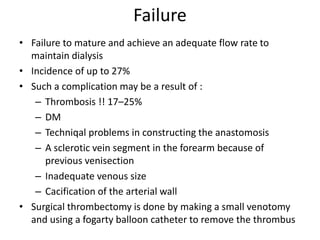
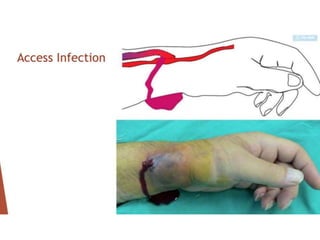
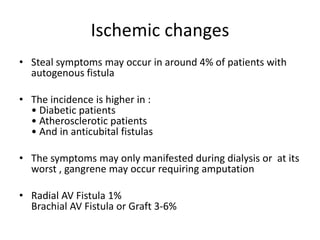
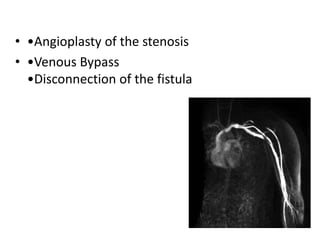
This document discusses surgical interventions for complications arising from arteriovenous fistulas (AVF), emphasizing their superiority over catheter access for dialysis patients. It outlines various complications, such as thrombosis, infection, and ischemic changes, along with appropriate surgical treatments for these issues. The importance of maintaining AVF patency and addressing complications before patient discharge is highlighted.