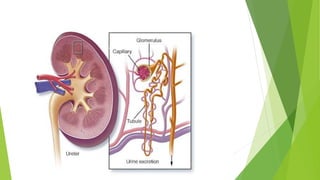
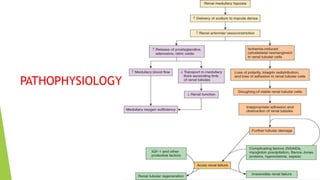
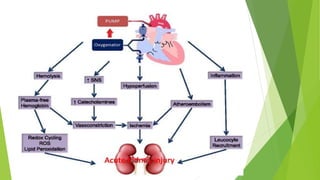
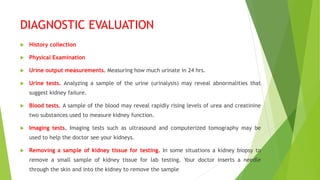
Acute renal failure, also known as acute kidney injury, is characterized by a sudden decline in kidney function, leading to waste accumulation in the blood. It commonly occurs in hospitalized patients and can result from various factors such as decreased blood flow, toxic substances, and urinary obstructions. Key symptoms include decreased urine output, fluid retention, and confusion, while management may involve fluid balancing, medications, or dialysis.