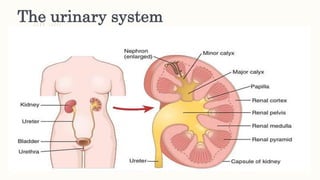
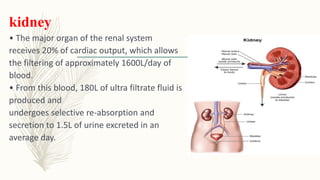
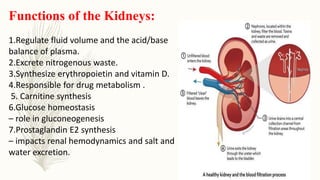
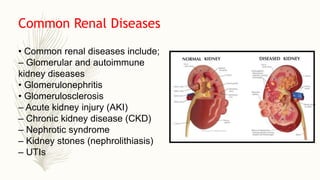
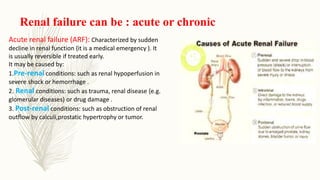
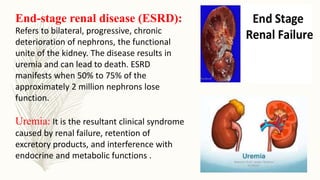
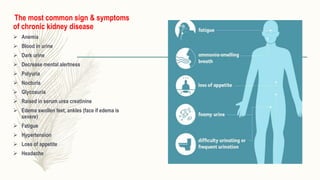
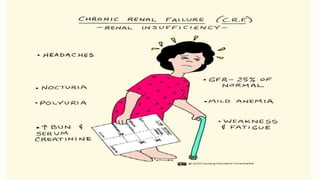
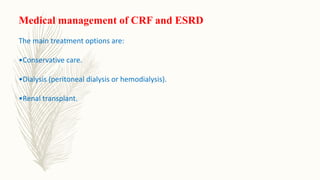
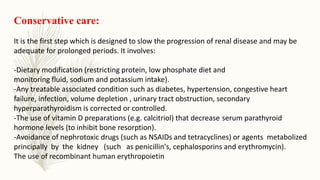
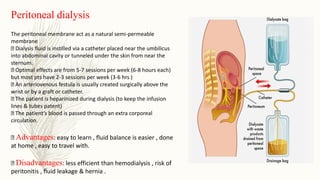
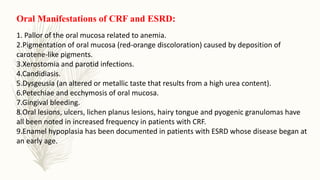
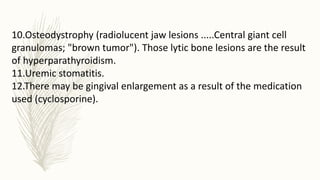
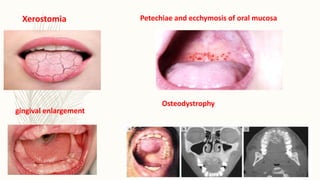
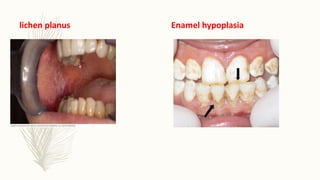
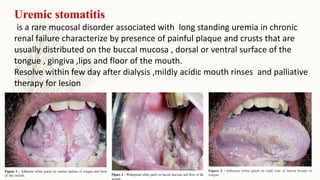
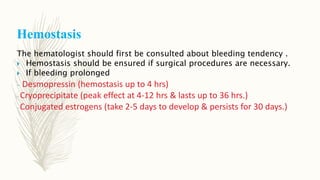
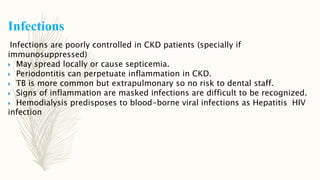
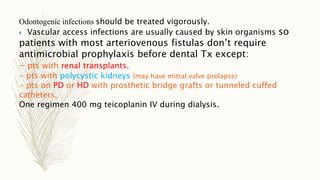
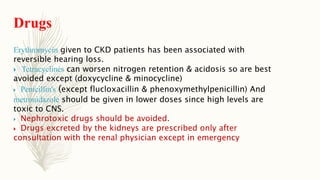
The document provides a comprehensive overview of the renal system, its functions, and common renal diseases such as chronic kidney disease (CKD) and acute kidney injury (AKI). It details the signs and symptoms of renal failure, the clinical features, diagnosis, and management options including conservative care, dialysis, and renal transplant. Additionally, the document discusses the implications of renal disease on dental care, highlighting the importance of routine oral examinations in affected patients.
![Renal disase [autosaved]](https://image.slidesharecdn.com/renaldisaseautosaved-200302093857/85/Renal-disase-autosaved-42-320.jpg)