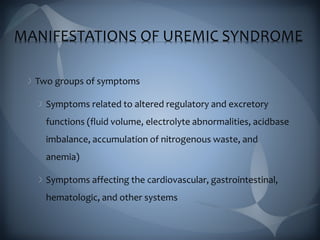
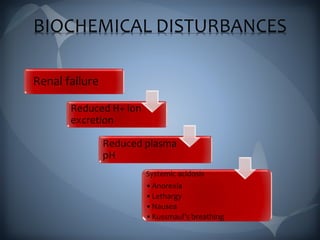
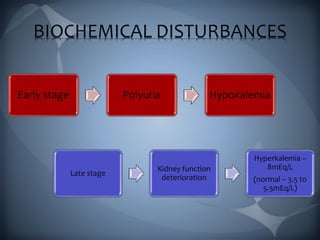
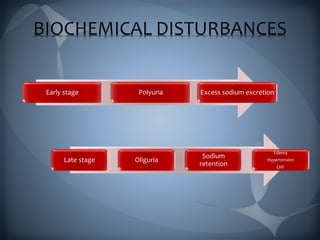
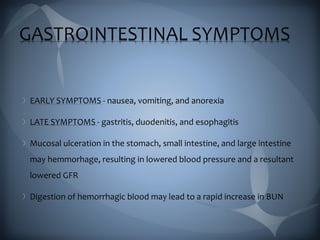
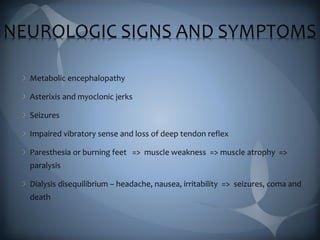
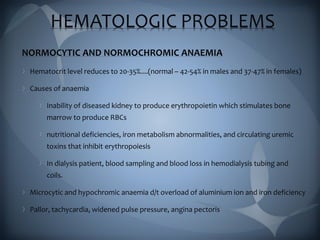
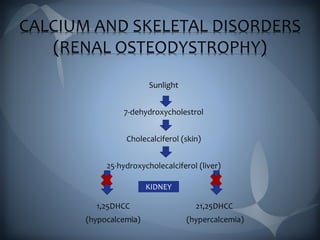
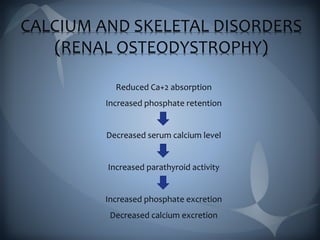
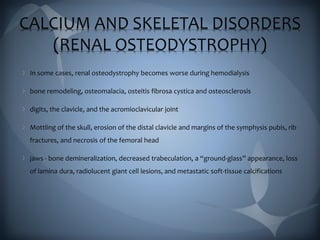
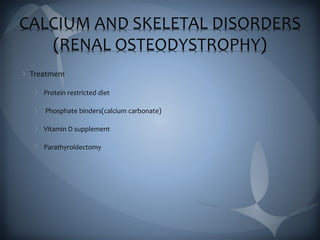
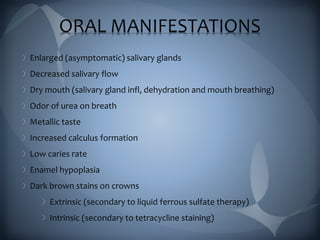
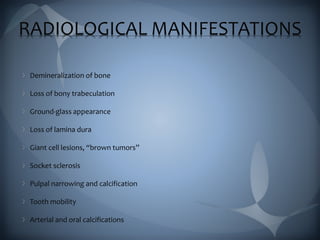
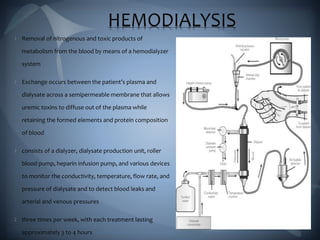
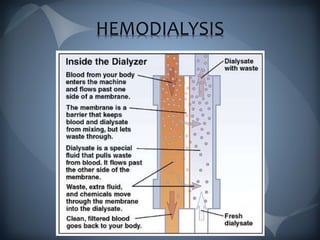
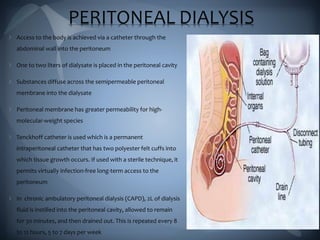
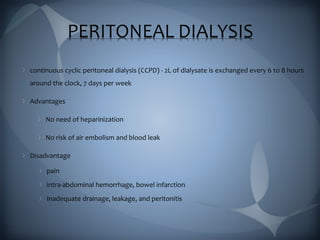
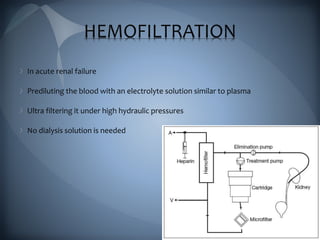
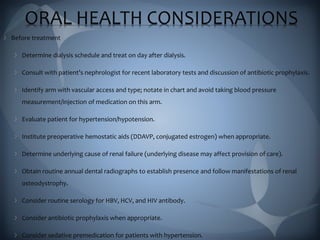
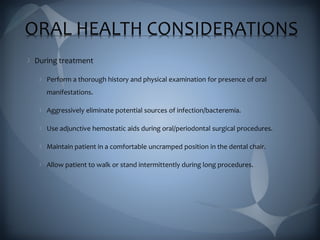
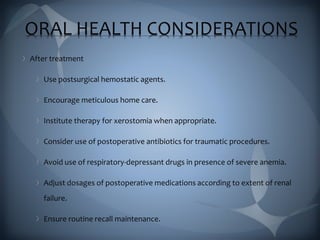
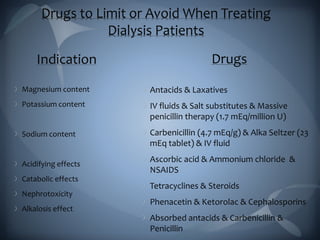
This document discusses the manifestations and complications of renal disease and uremic syndrome. It covers the biochemical disturbances that occur like acidosis, electrolyte abnormalities, and fluid retention. Symptoms affecting various organ systems are described, like gastrointestinal issues, neurological signs, hematological problems, and skeletal disorders. Medical management including conservative therapies focusing on diet, medications, and preparing for dialysis are outlined. The two main types of renal replacement therapy, hemodialysis and peritoneal dialysis, are explained in detail. Oral health considerations for patients undergoing treatment are also noted.