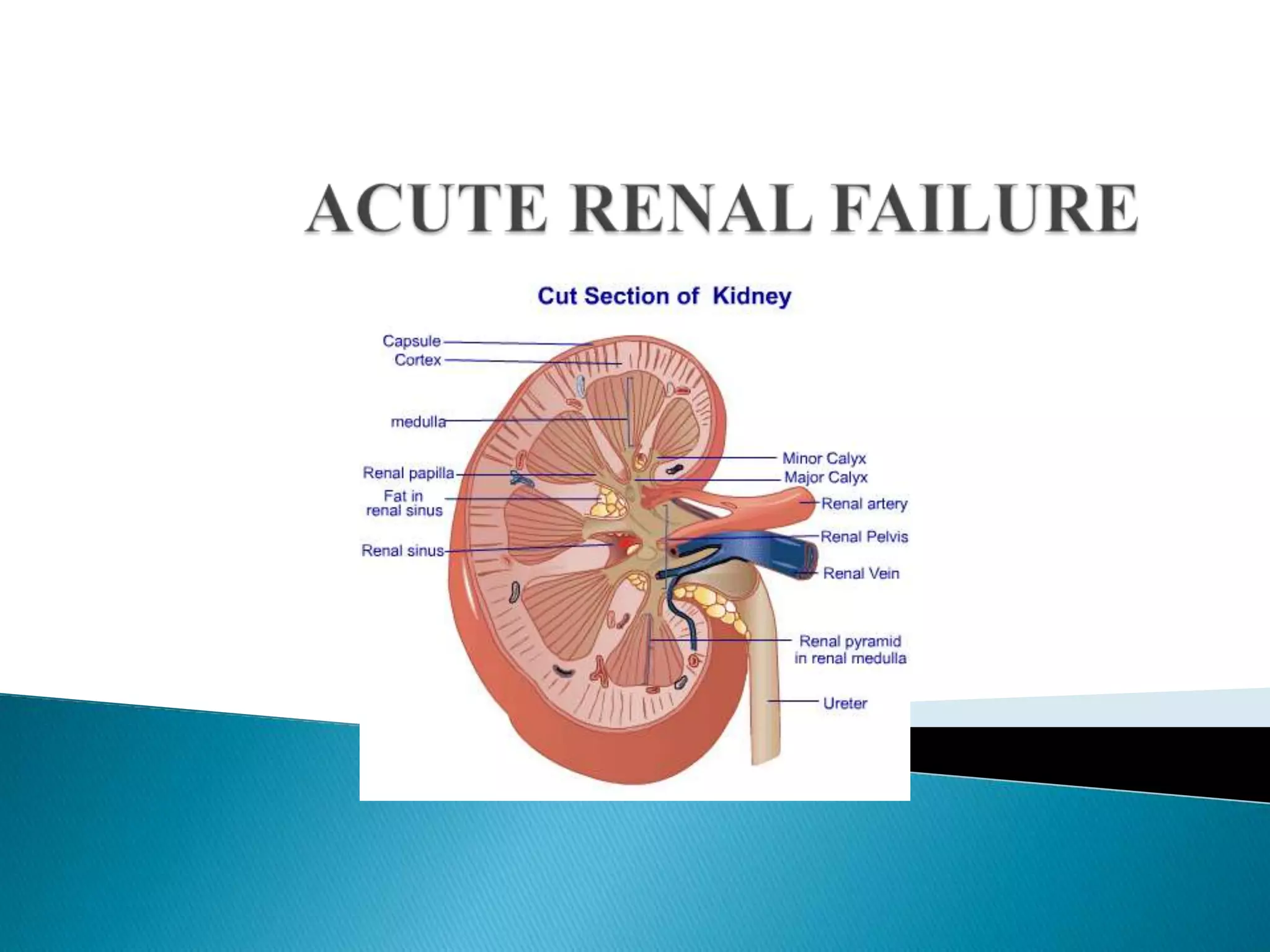
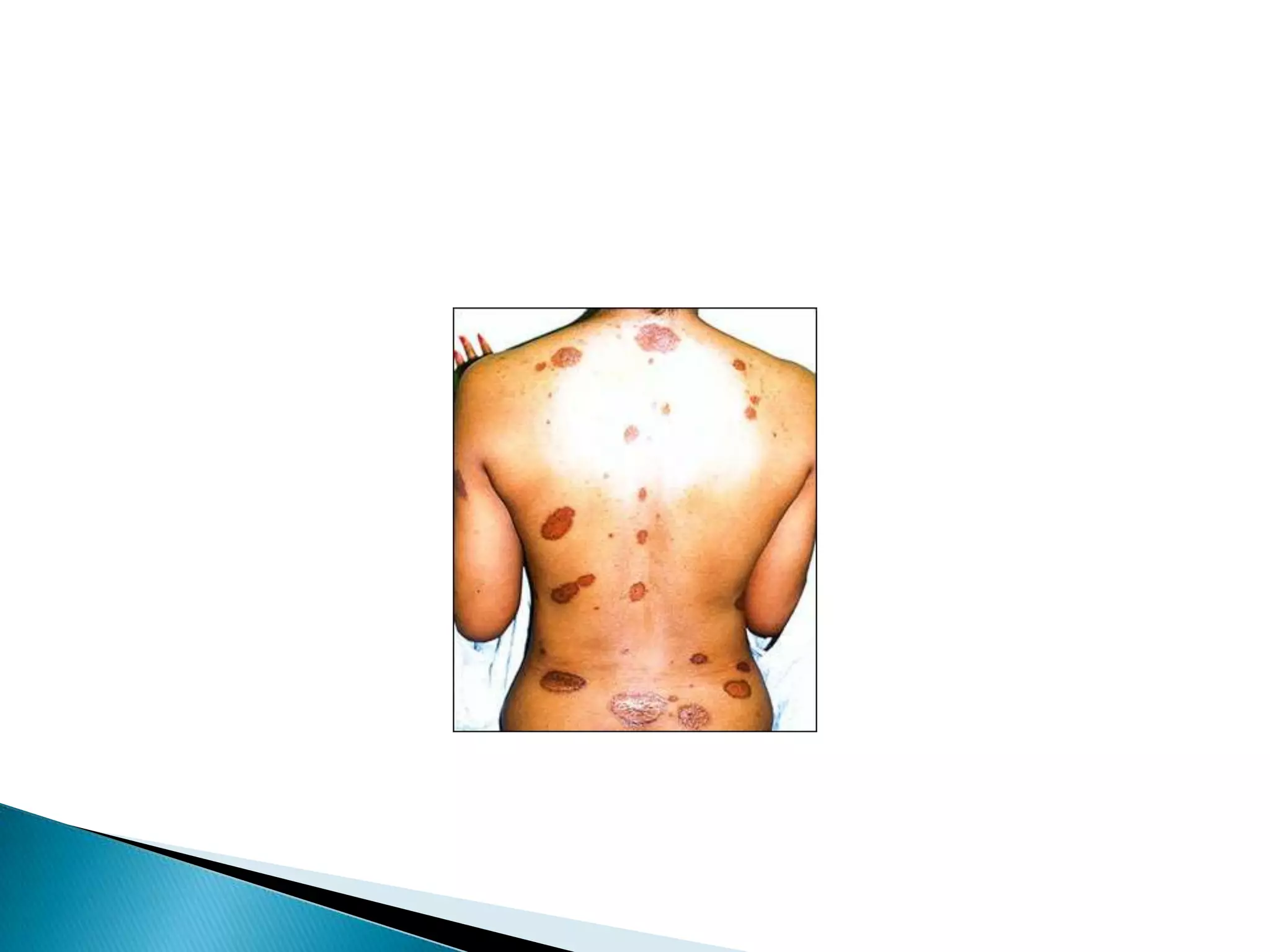
Acute renal failure is a sudden reduction in kidney function that results in waste accumulating in the blood. It can be caused by problems affecting blood flow to the kidneys like dehydration, blood loss from major surgery or burns, or kidney problems preventing proper filtration. Symptoms include reduced urination, swelling, fatigue, and shortness of breath. Treatment focuses on fluid balance, electrolytes, nutrition, and preventing complications like infection that can further stress the kidneys.