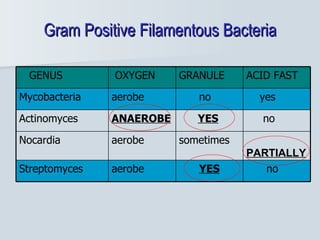
1. Actinomyces and Nocardia are filamentous, Gram-positive bacteria found in the environment and as normal flora in humans.
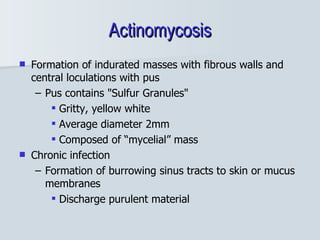
2. Actinomyces causes cervicofacial and abdominal actinomycosis in humans through tissue invasion following trauma or medical procedures. Diagnosis involves identifying sulfur granules in biopsy specimens.
3. Nocardia is an opportunistic pathogen that can cause pulmonary, cutaneous, or disseminated nocardiosis through inhalation or skin inoculation. It is an important cause of infection in immunocompromised individuals.