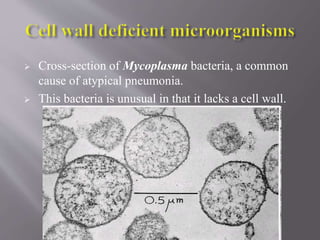
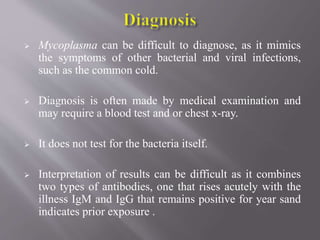
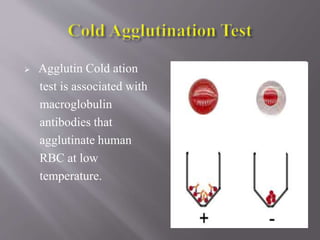
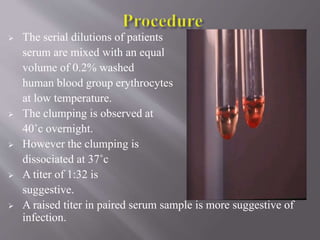
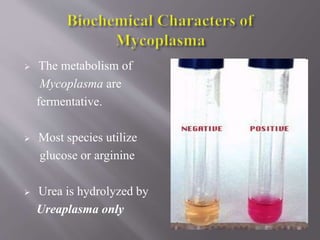
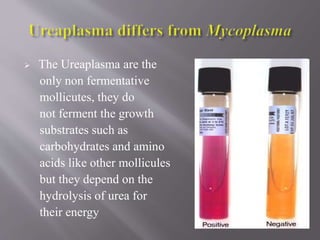
Mycoplasma are unique prokaryotes that lack a cell wall. They can cause respiratory infections like pneumonia that spread through coughing and sneezing. Symptoms include cough, fatigue, and weakness. Diagnosis involves blood tests to detect antibodies. Treatment involves antibiotics like erythromycin and doxycycline. Prevention relies on good hygiene practices.