1. Health promotion and disease prevention strategies must be individualized for older adults due to age-related changes, life expectancy, and personal preferences.
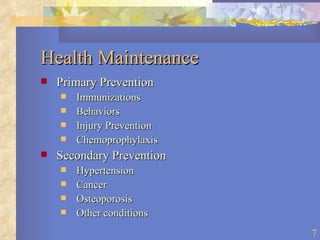
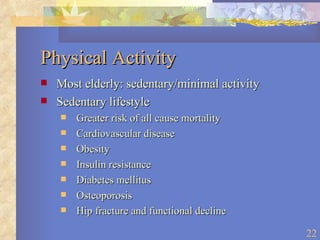
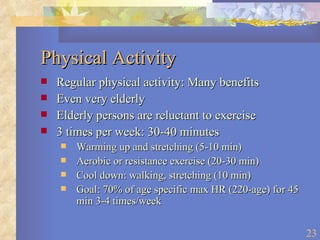
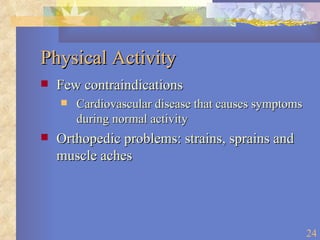
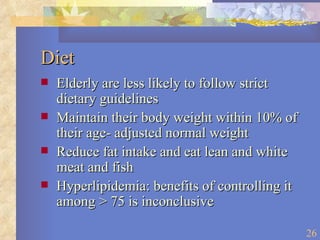
2. Immunizations against influenza, pneumonia, and tetanus are effective prevention methods supported by evidence in geriatrics. Regular physical activity and a healthy diet also promote wellness.
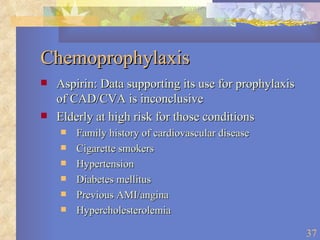
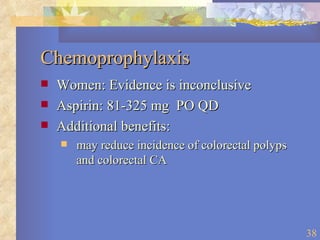
3. More research is needed to determine the effectiveness and optimal application of many prevention strategies in older populations due to limited evidence and the heterogeneity of aging. Preventive interventions should consider overall health status and goals of care.