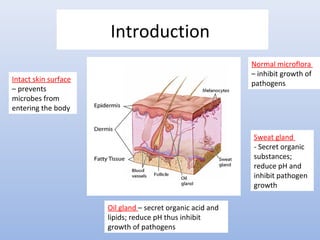
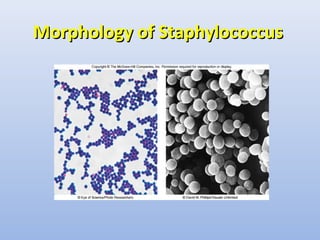
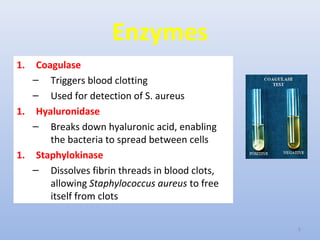
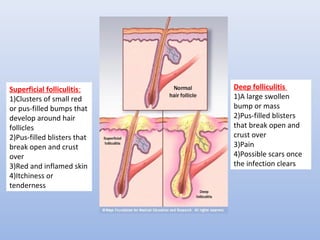
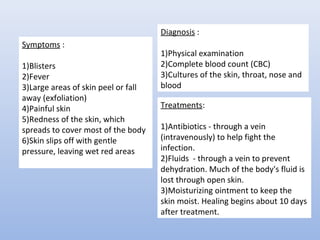
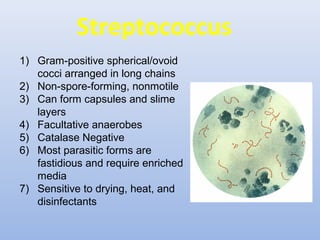
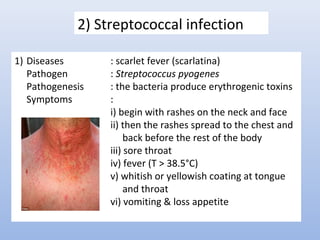
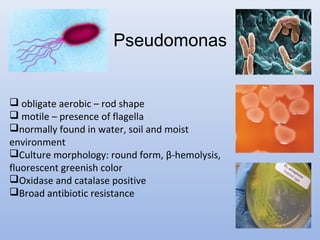
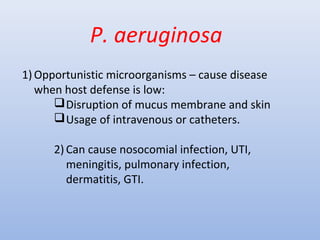
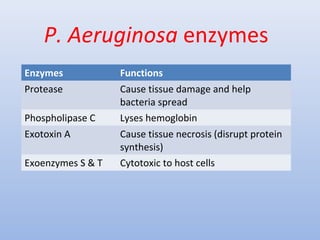
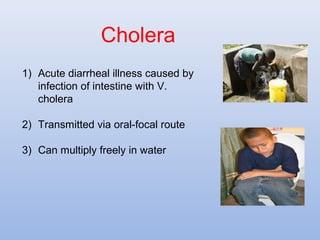
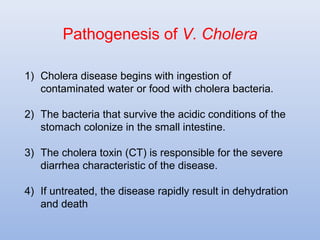
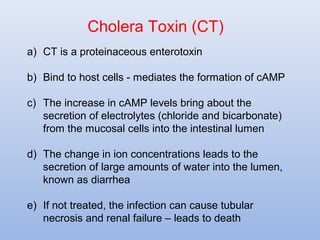
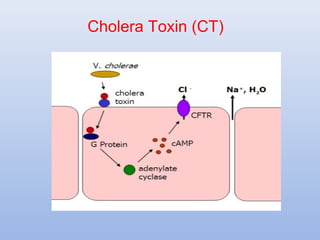
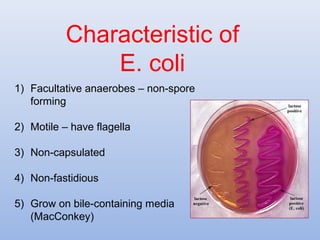
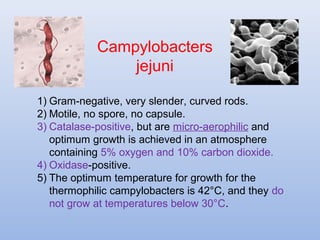
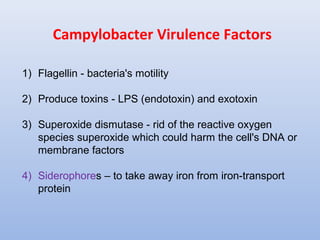
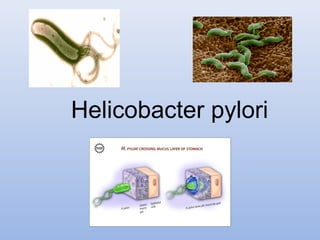
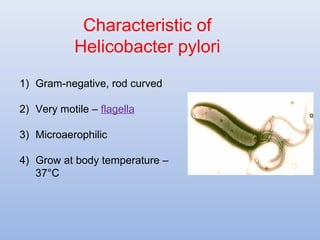
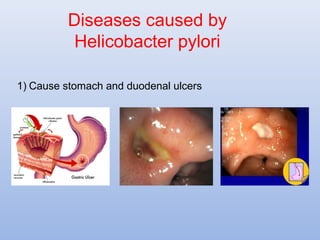
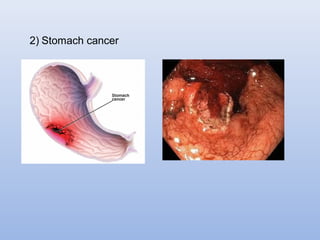
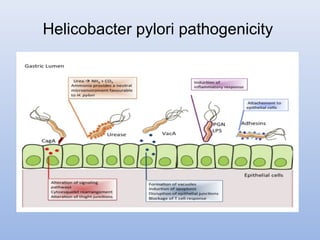
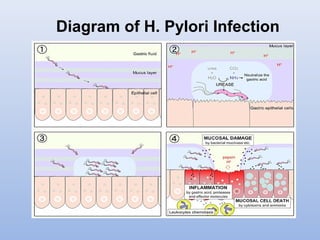
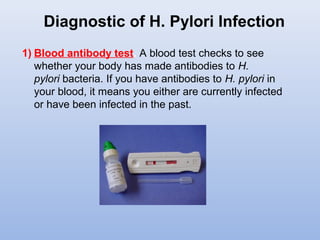
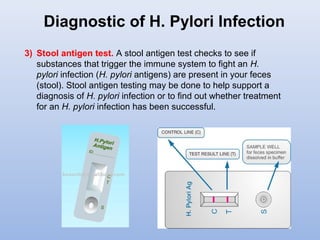
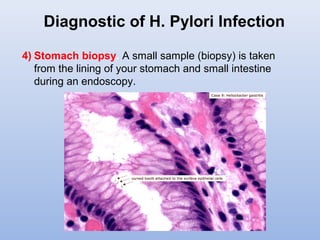
This document provides an overview of bacterial skin diseases and infections. It discusses several gram-positive bacteria like Staphylococcus and Streptococcus that can cause infections. It describes common skin infections from Staphylococcus like folliculitis and boils. It also covers Streptococcus and the skin infection of scarlet fever. The document further discusses gram-negative pathogens such as Pseudomonas, Vibrio, E. coli, Campylobacter, Helicobacter, and Neisseriae that can infect the skin. It provides details on diseases associated with these bacteria and their characteristics, transmission, pathogenesis and symptoms.