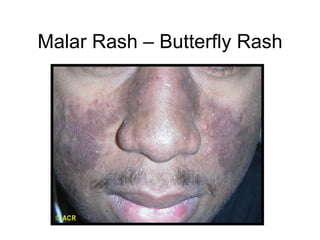
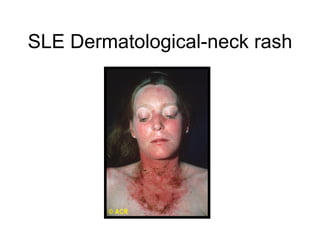
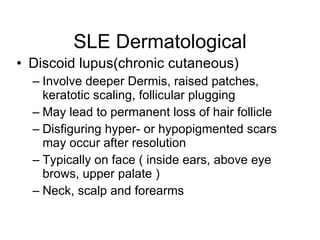
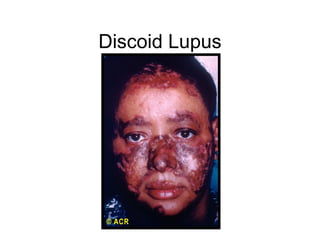
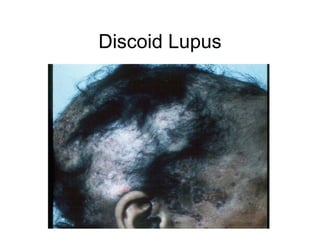
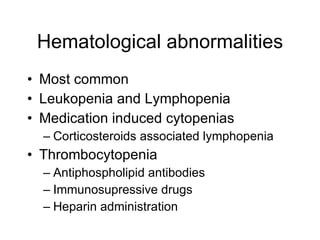
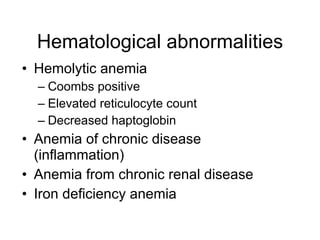
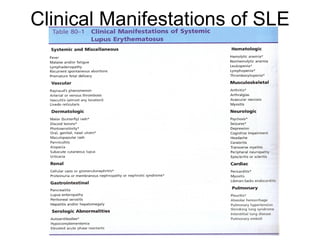
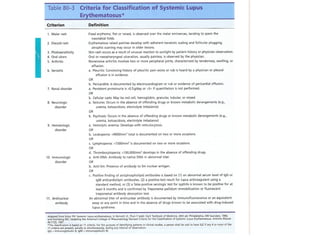
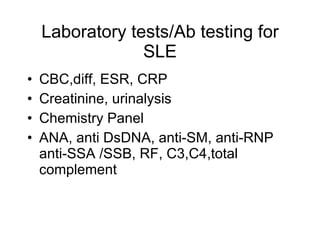
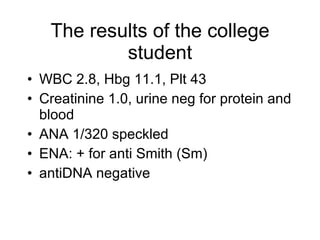
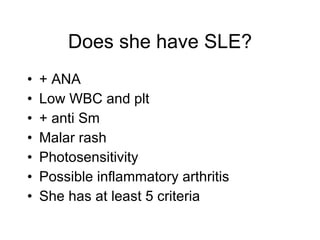
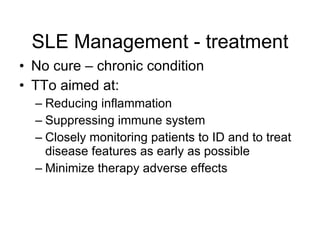
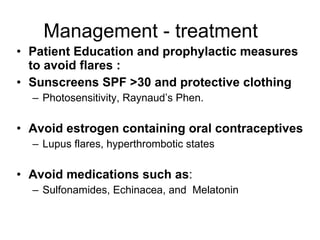
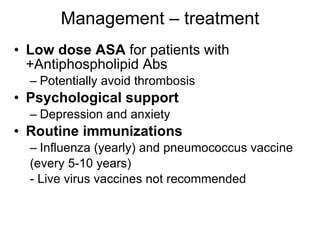
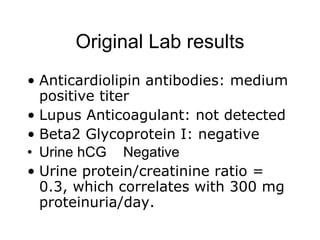
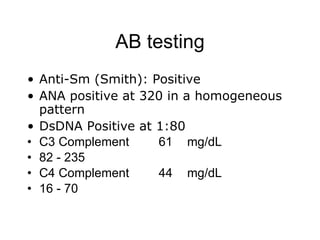
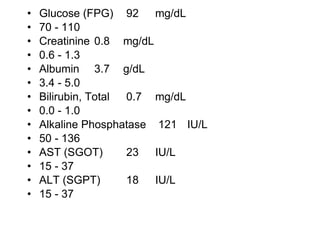
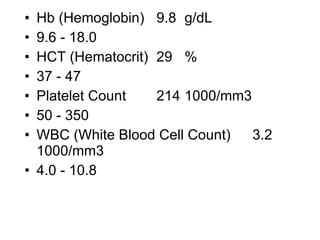
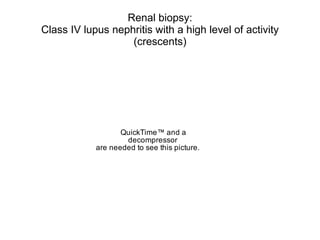
A 22-year-old college student presents with symptoms including a malar rash, photosensitivity, arthritis, fatigue, and hair loss. Laboratory tests show a positive ANA, positive anti-Smith antibody, and low white blood cell and platelet counts. This constellation of clinical features and laboratory results makes systemic lupus erythematosus the most likely diagnosis for the patient.