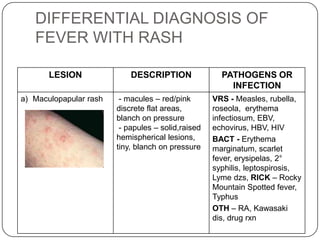
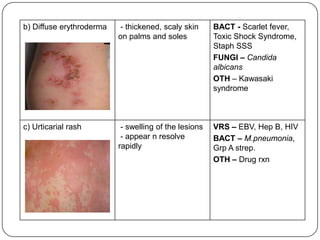
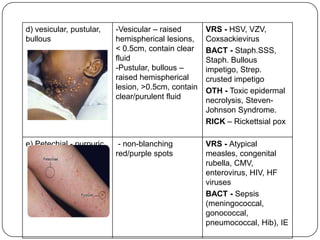
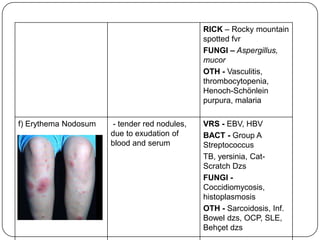
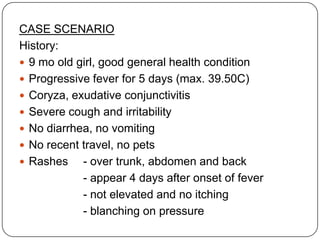
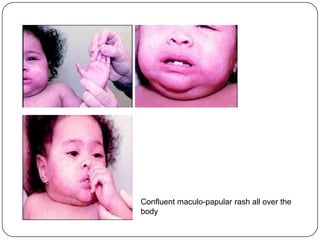
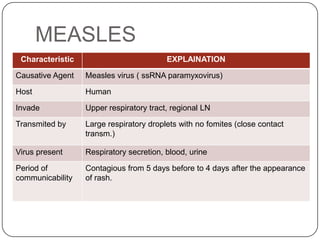
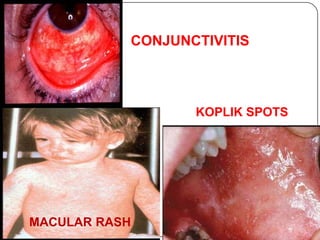
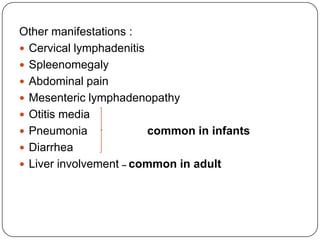
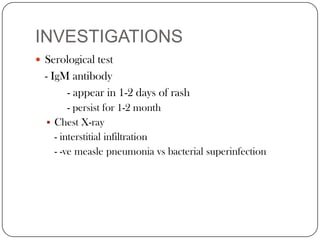
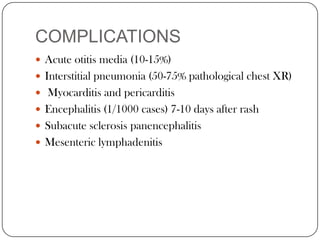
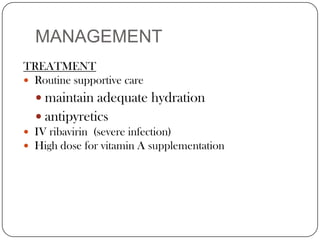
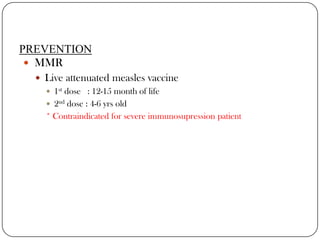
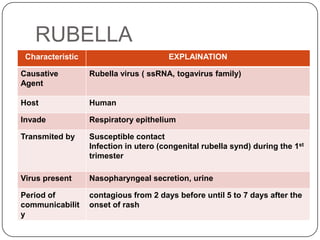
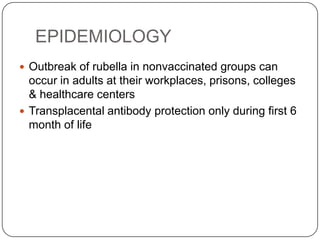
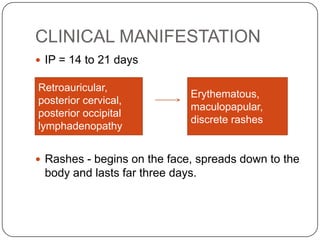
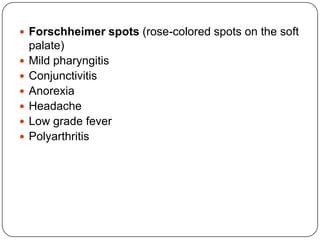
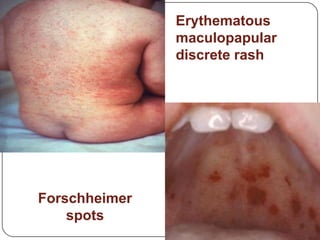
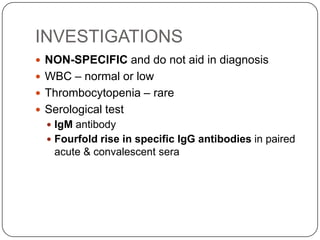
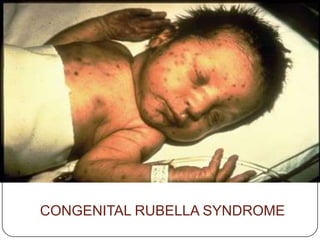
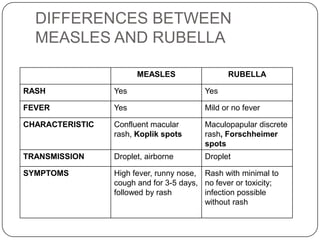
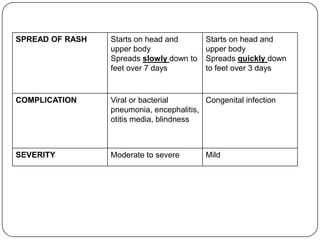
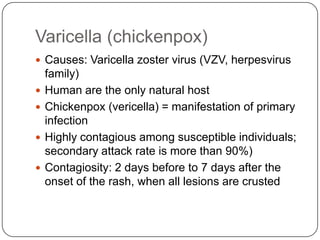
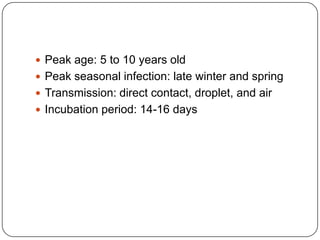
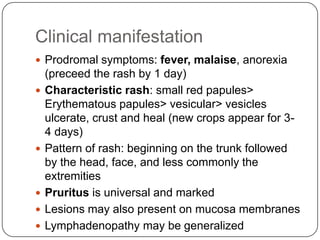
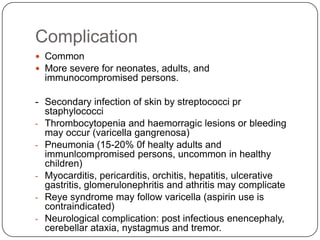
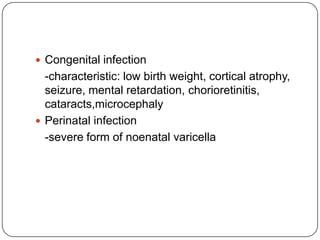
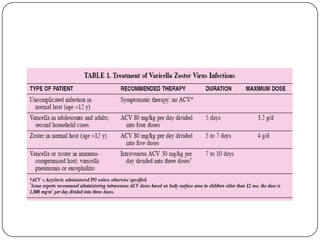
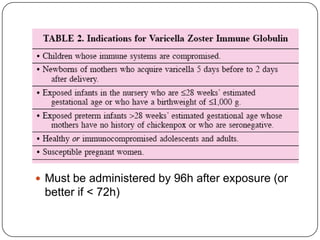
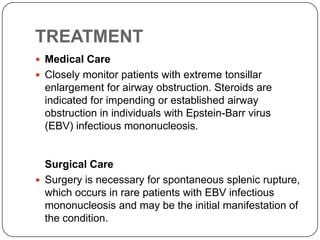
This document discusses several pediatric infectious diseases that present with fever and rash: measles, rubella, varicella, and hand, foot and mouth disease. It provides details on the causative agents, clinical manifestations, investigations, treatment, prevention, and complications of each disease. A case scenario is also presented describing a 9-month-old girl presenting with fever, rash, cough and conjunctivitis consistent with measles. Differential diagnoses and distinguishing features between measles and rubella are also summarized.