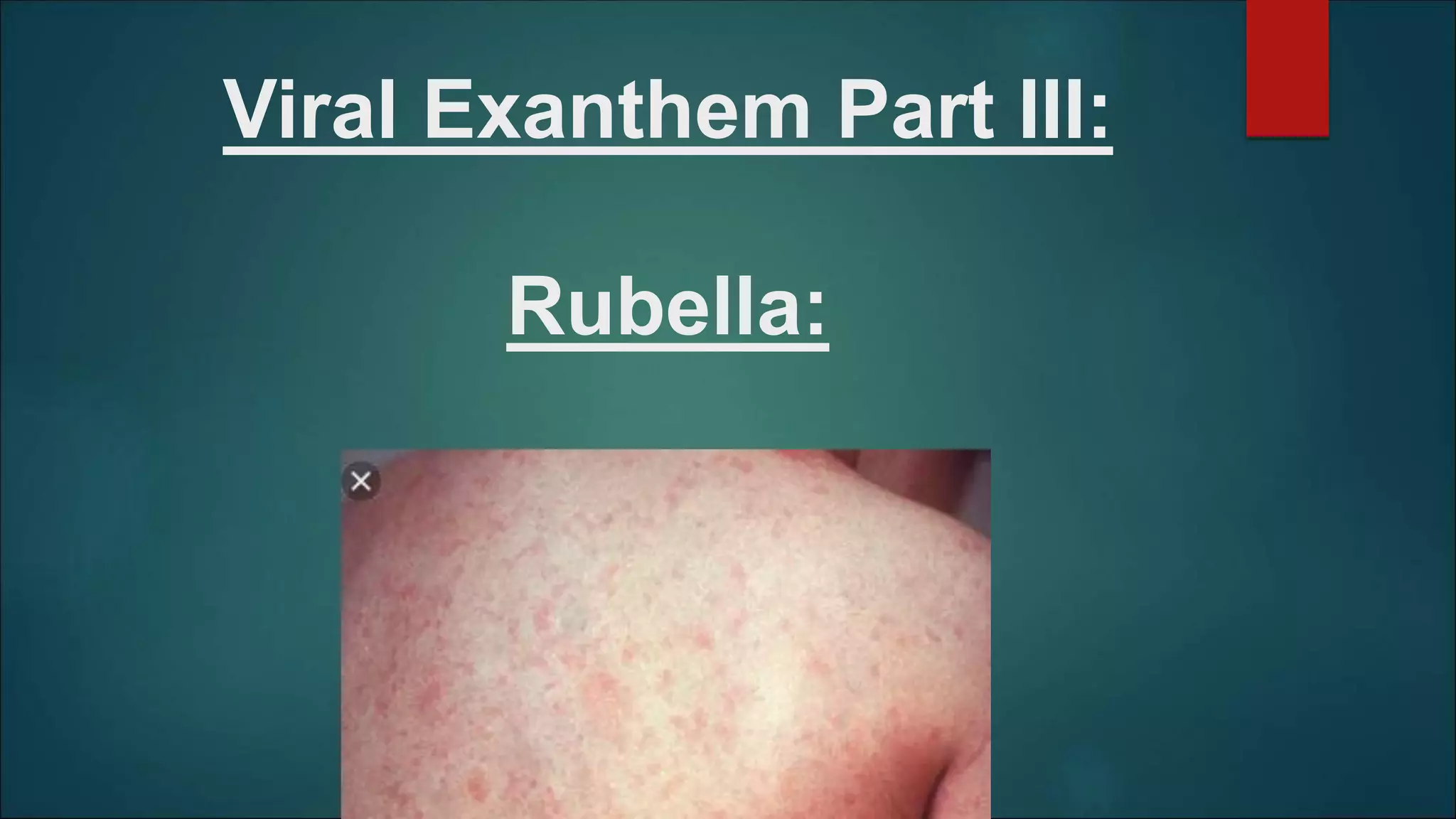
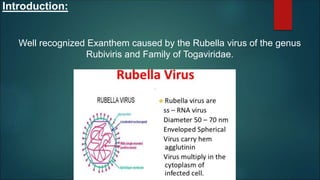
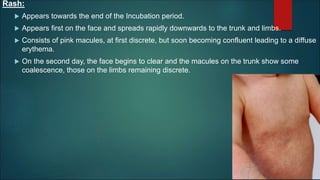
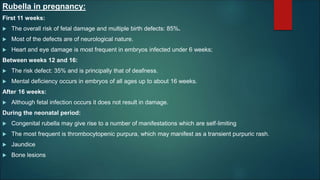
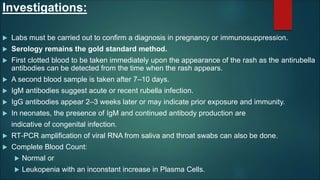
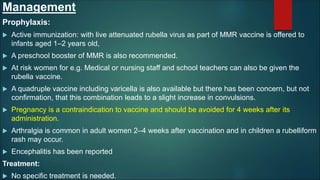
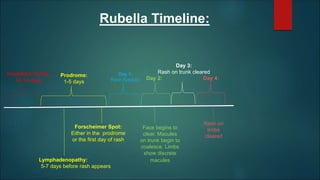
Rubella, caused by the rubella virus, primarily affects older children and young adults, with its incidence peaking during spring. The disease features a 14-day incubation period, a characteristic rash, and complications such as arthritis and fetal damage in pregnant women. Diagnosis involves lab confirmation and serology, while management focuses on vaccination and monitoring, as no specific treatment is required.