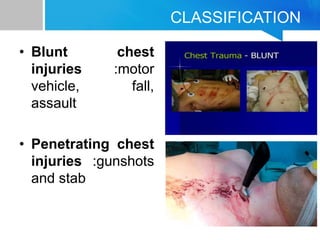
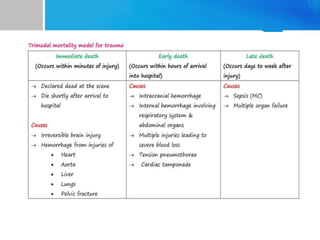
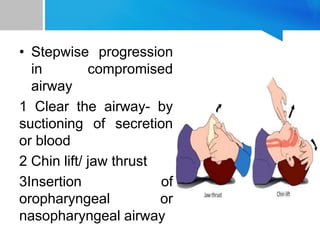
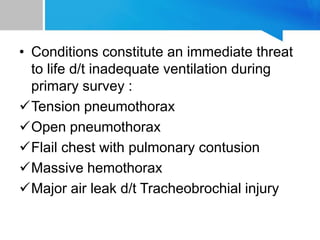
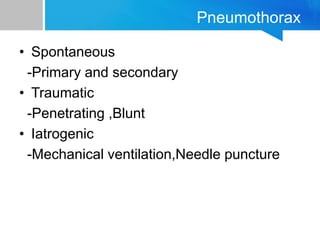
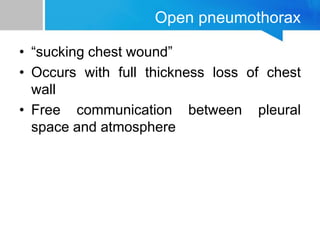
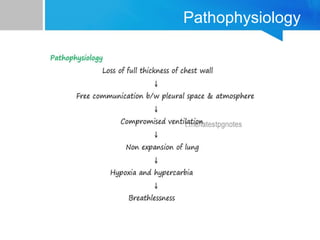
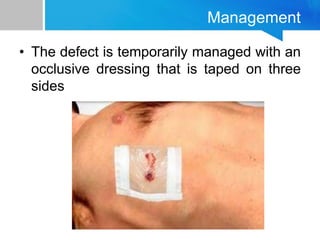
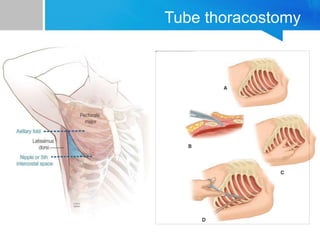
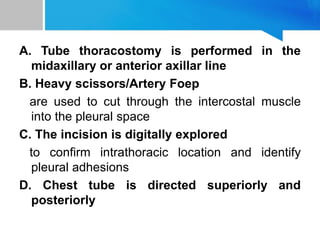
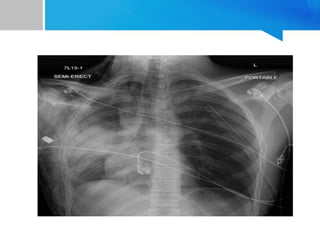
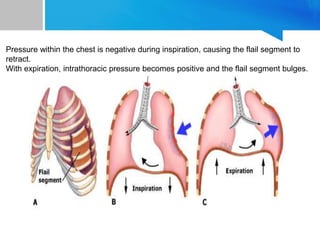
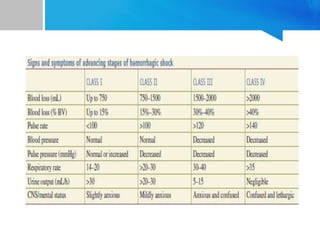
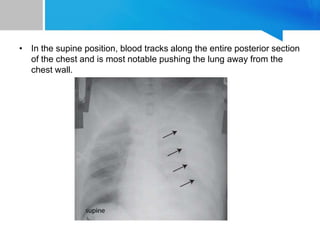
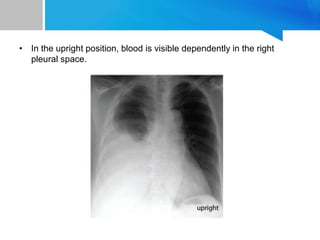
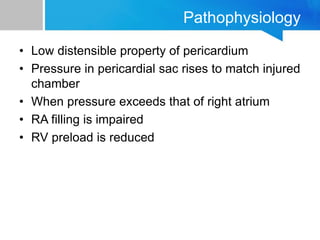
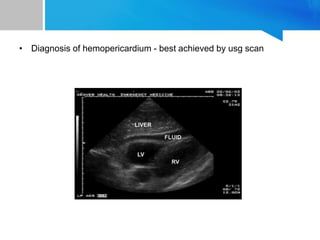
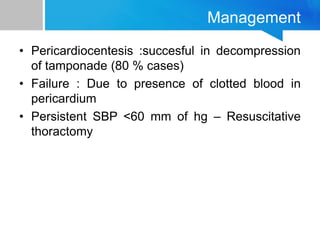
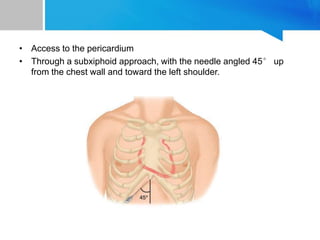
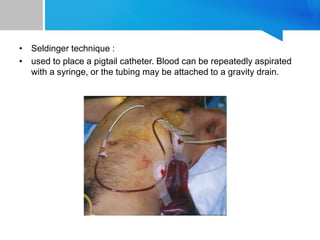
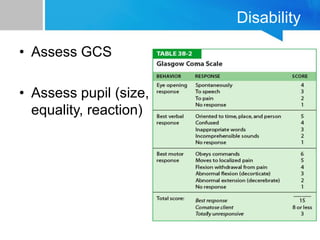
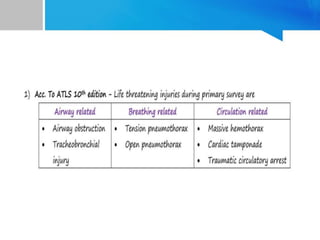
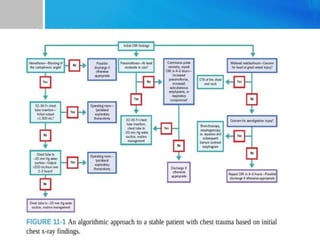
This document provides an overview of chest trauma. It begins by defining trauma and injuries, noting that mechanical forces are most common. Chest injuries account for 20-25% of trauma deaths. Blunt and penetrating injuries are classified. Motor vehicle collisions are a leading cause of chest trauma. The ATLS principles focus on rapid assessment and management to reduce morbidity and mortality. The primary survey addresses airway, breathing, circulation, disability and exposure. Specific injuries like pneumothorax, hemothorax, flail chest and cardiac tamponade are discussed in terms of pathophysiology, diagnosis and management. Tube thoracostomy and thoracotomy are mentioned as approaches to drainage for certain injuries.