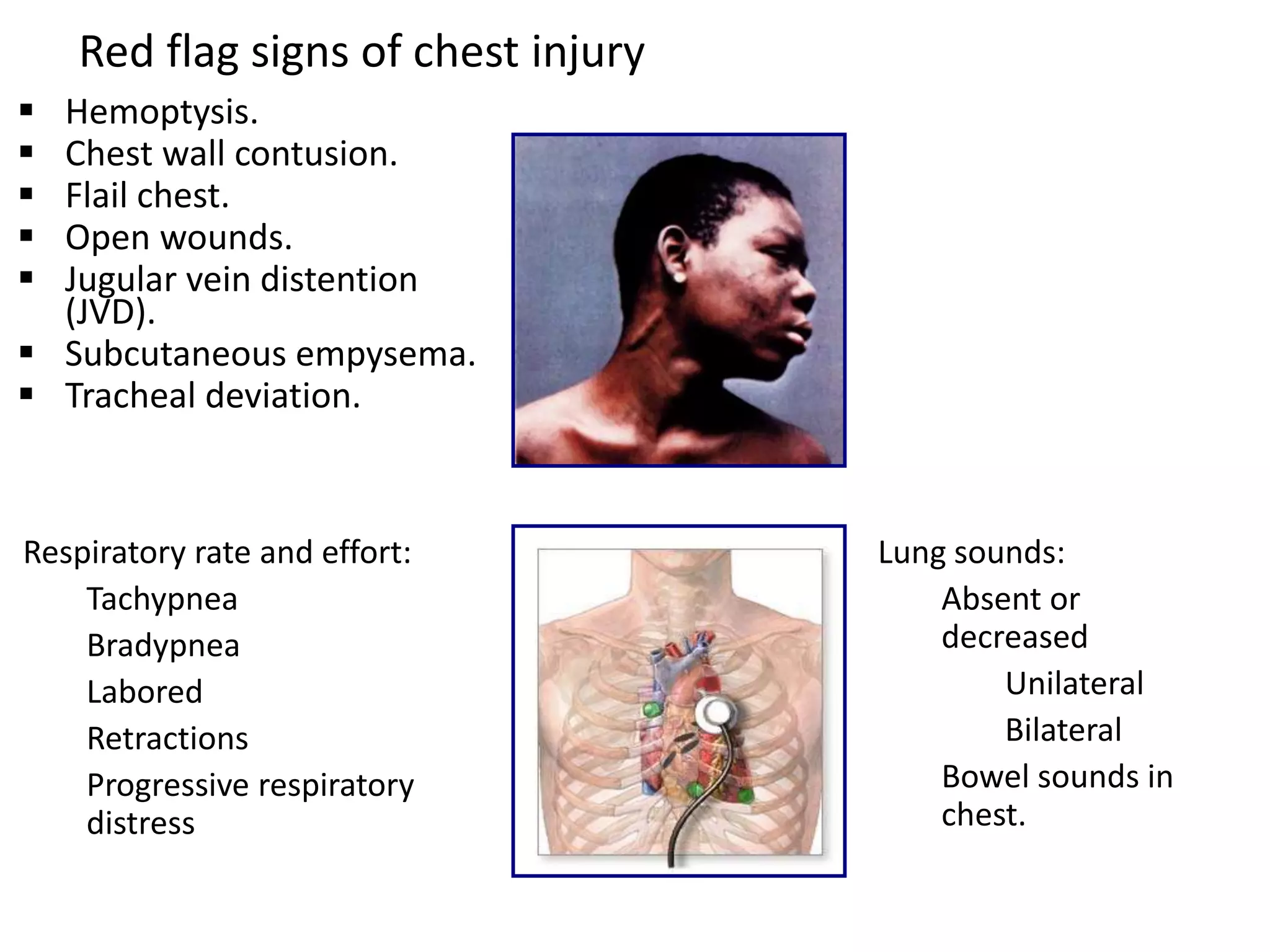
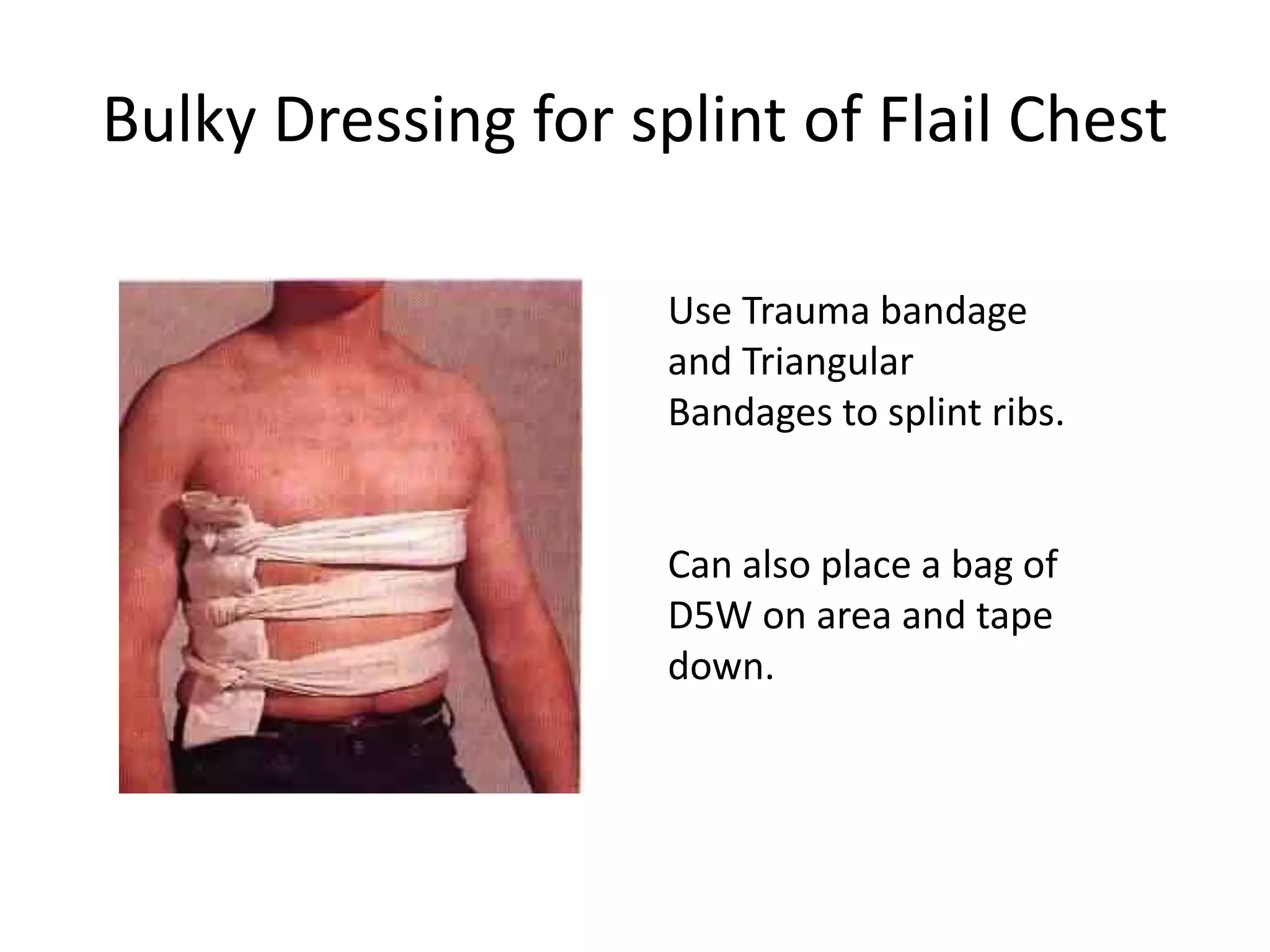
This document provides information on the anatomy of the chest and causes, symptoms, diagnosis, and treatment of various types of chest injuries. It discusses conditions like airway obstruction, flail chest, sucking chest wounds, hemothorax, tension pneumothorax, and cardiac tamponade. For each condition, it outlines the pathophysiology, diagnostic indicators, and emergency treatment procedures like needle decompression and pericardiocentesis. The document emphasizes the importance of stabilizing life-threatening conditions in the primary survey and provides details on emergency department management of chest trauma.







![• *chest -[33.33%] in RTA cases.
• The majority of such injuries may be diagnosed
with relatively simple tests such as chest
radiographs.
• *JRFMT-2016Month :December Volume :2
Issue:2 Page :8-13](https://image.slidesharecdn.com/chesttrauma222-170315112756/75/Chest-trauma-Emergency-Medicine-8-2048.jpg)