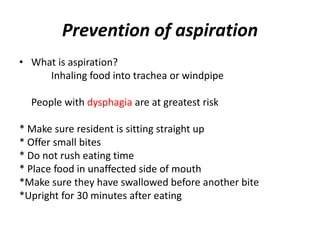
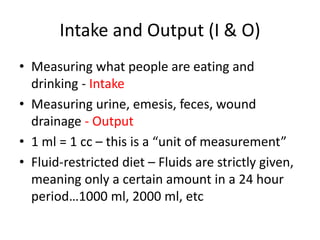
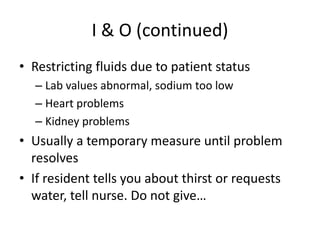
Good nutrition is important for healing, stress tolerance, and metabolism. The elderly have different nutritional needs than younger people due to slower metabolism and changes in digestion. Factors like illness, dentition, taste changes, and depression can contribute to nutritional deficits. Facilities must provide nutritious and culturally appropriate meals while accommodating special diets and assisting residents who have difficulties eating or swallowing to prevent aspiration. Intake and output must be carefully monitored and recorded to prevent dehydration or fluid overload.