A therapeutic diet is a meal plan prescribed to treat a medical condition. It controls certain foods/nutrients and is planned by a dietician under physician guidance. Therapeutic diets aim to maintain good nutrition, correct deficiencies, adjust food intake based on ability to metabolize nutrients, and change body weight if needed. Modifications can be qualitative like restricting/excess of nutrients, or quantitative like changing consistency or meal frequency/composition. Common hospital diets include clear liquids, full fluids, soft foods, and normal diets for various indications.
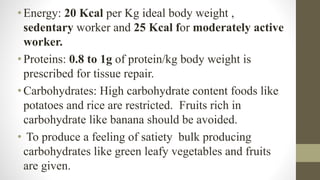
![• : Dietary Guidelines
• Soups prepared from vegetables/pulses without added fats
or starch
• Salads prepared using raw tomato, cucumber, cabbage,
capsicum, radish, carrots, sprouted green gram or bengal
grams
• High calorie fruits like mangoes, bananas and dry fruits
should be avoided
• : Avoid concentrated sugar, honey, ice cream, puddings,
chocolate, candy etc. Alcoholic beverages to be avoided.
• ] : Avoid snacks between meals](https://image.slidesharecdn.com/presentationtherapeuticdiet-1-230925100142-da3f4e8f/85/Presentation-therapeutic-diet-1-pptx-33-320.jpg)