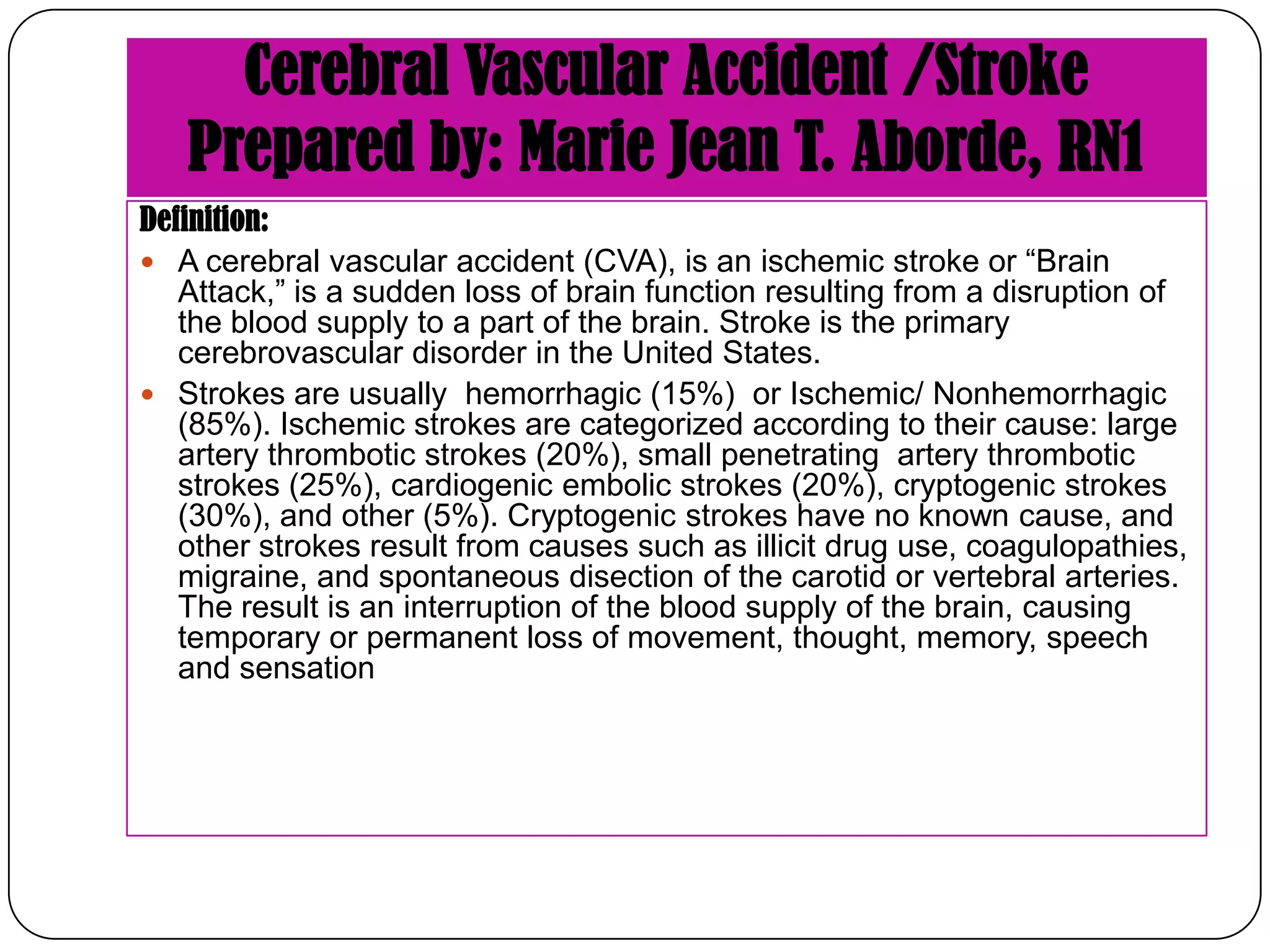
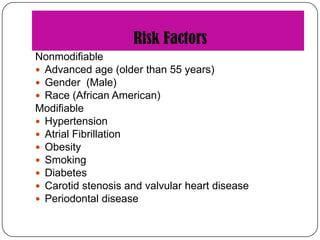
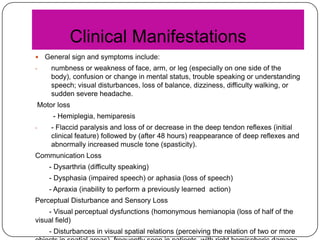
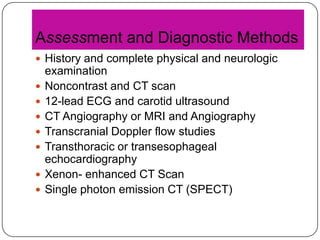
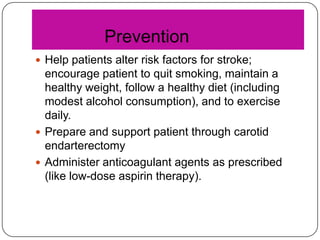
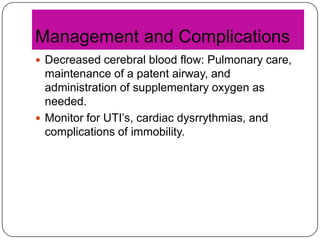
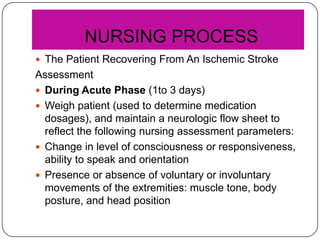
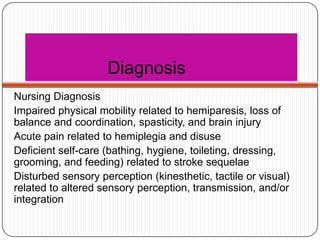
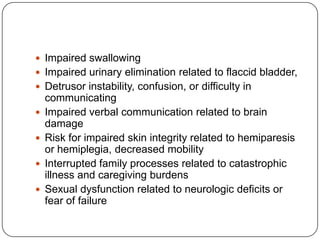
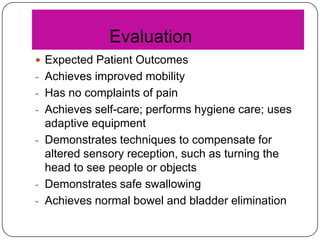
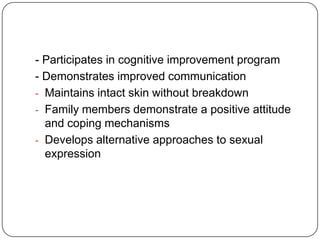
This document defines and describes cerebral vascular accidents (strokes). It notes that strokes are usually hemorrhagic or ischemic, and lists risk factors such as age, gender, hypertension, atrial fibrillation, and diabetes. Clinical manifestations include motor deficits, communication problems, sensory disturbances, and cognitive impairments. Diagnosis involves imaging tests and physical exams. Prevention focuses on modifying risk factors. Treatment includes thrombolytics, anticoagulants, managing complications, and rehabilitation to achieve goals like improved mobility and communication.