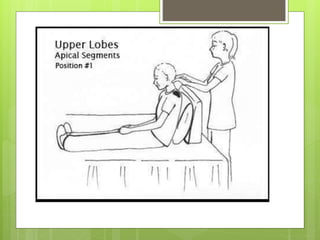
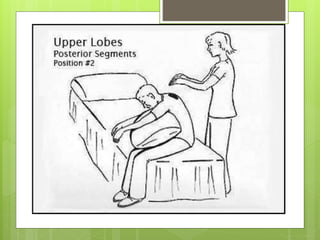
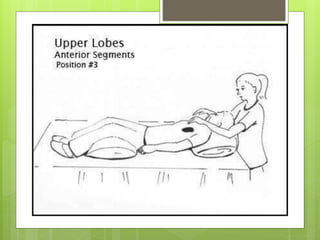
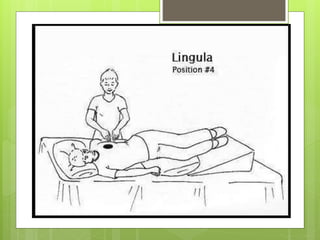
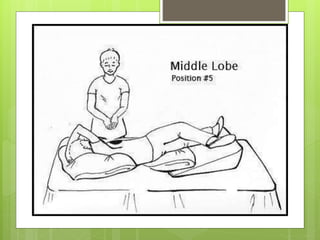
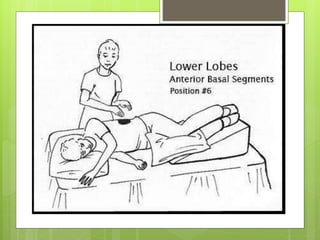
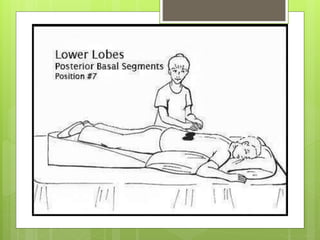
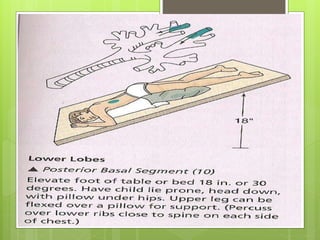
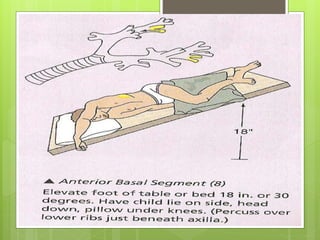
Postural drainage is a technique used to clear secretions from the lungs by placing patients in positions that utilize gravity. It involves tilting or propping patients at angles to drain secretions from the lungs into the central airways. Manual techniques like percussion, vibration, and shaking are used alongside positioning to loosen secretions and enhance their removal. Postural drainage is effective for conditions with increased mucus production and is commonly used for patients who have difficulty coughing up secretions due to illness, surgery, or prolonged bed rest.