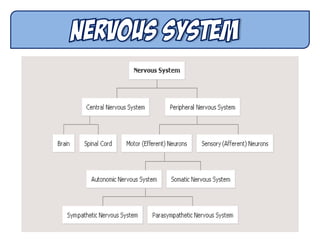
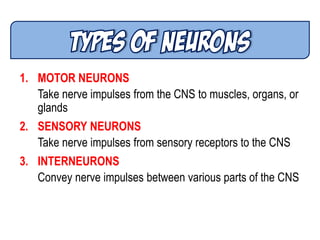
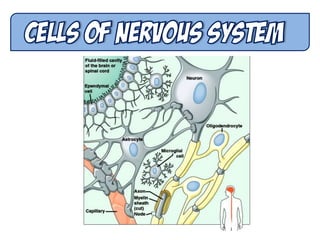
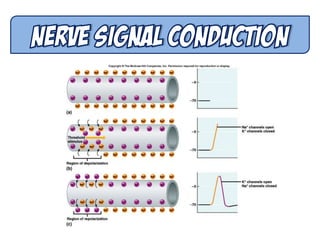
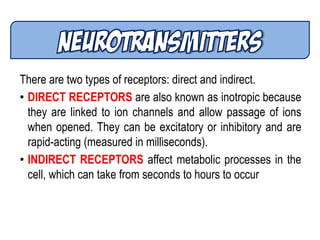
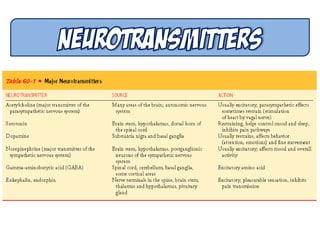
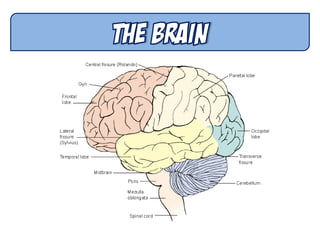
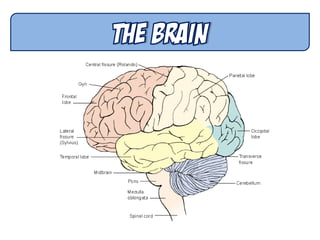
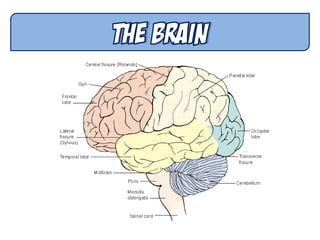
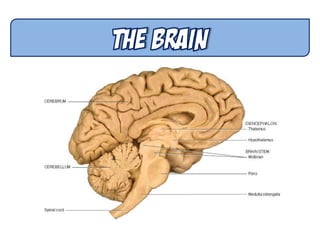
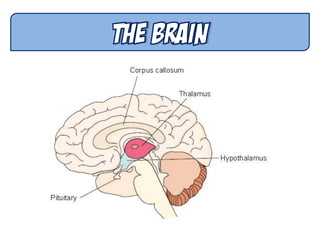
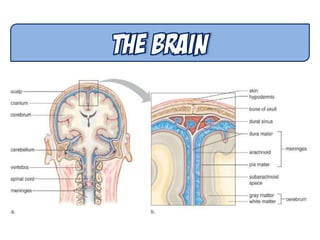
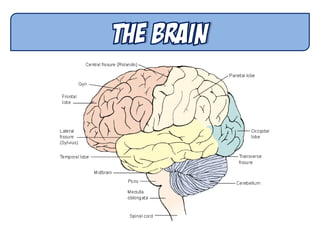
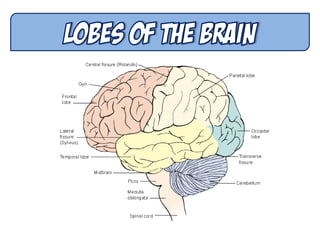
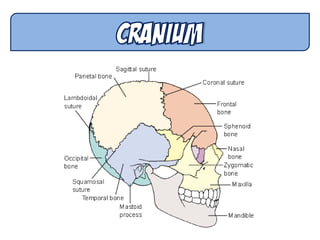
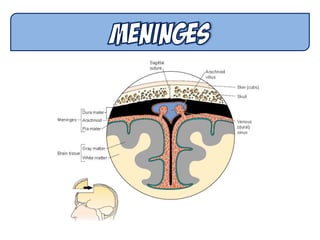
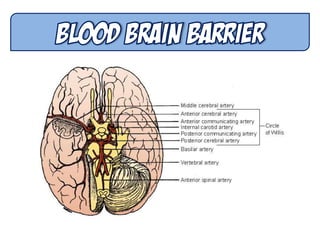
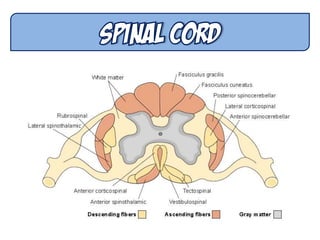
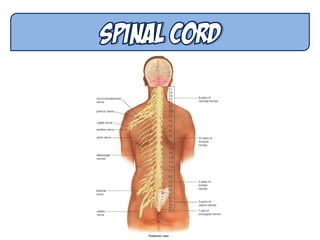
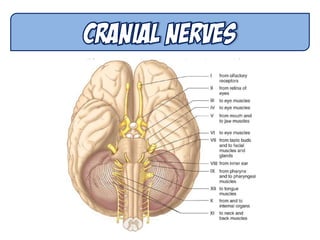
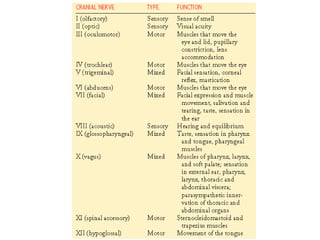
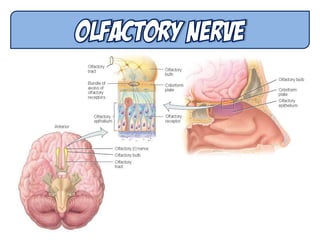
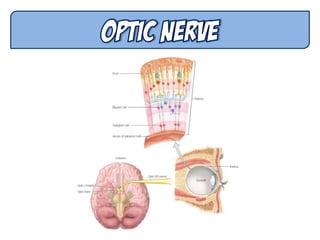
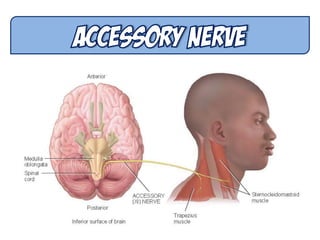
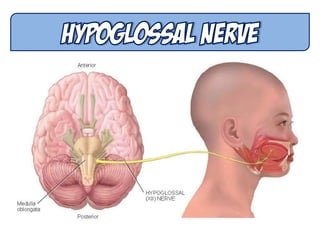
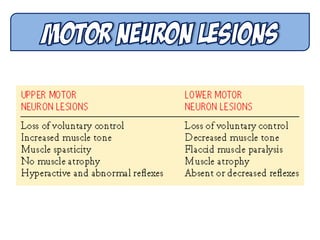
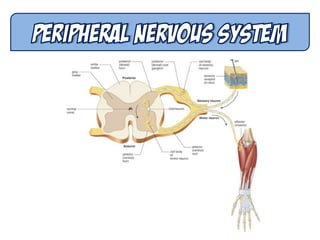
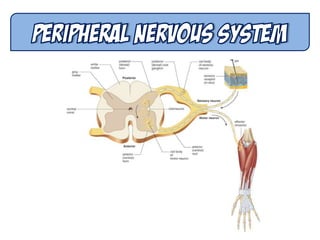
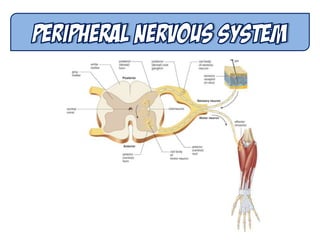
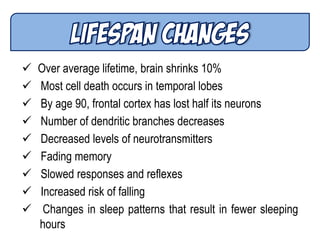
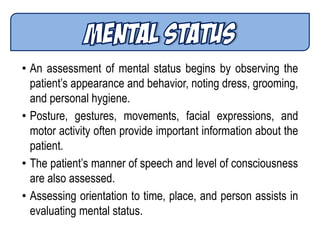
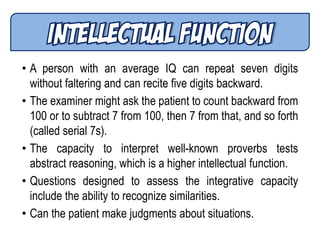
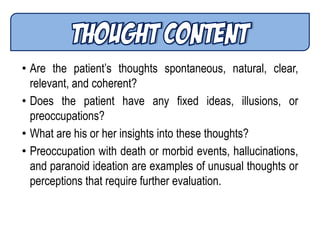
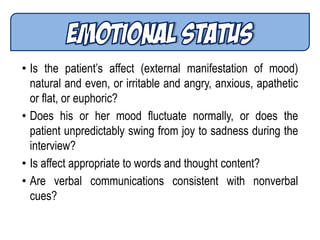
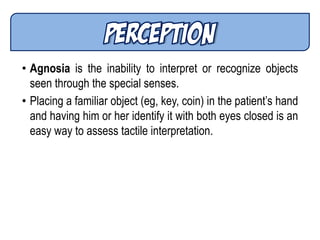
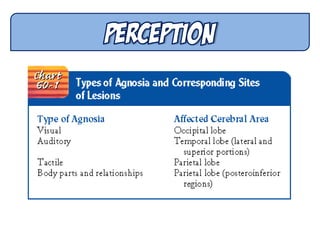
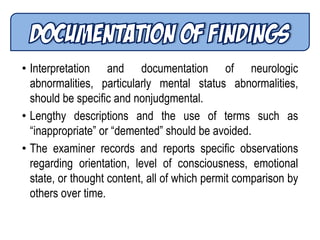
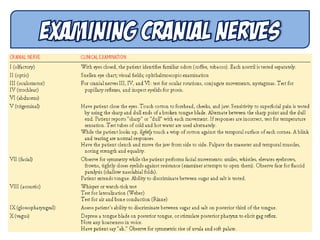
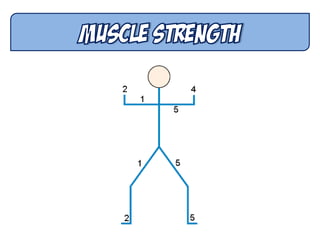
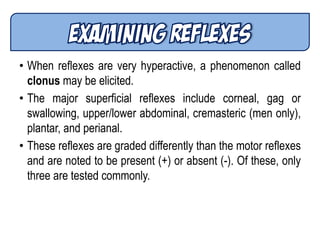
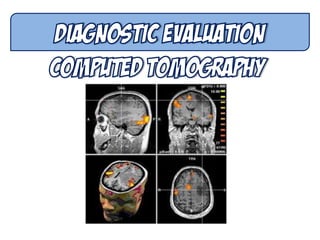
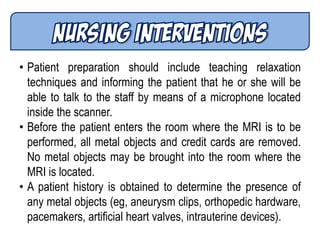
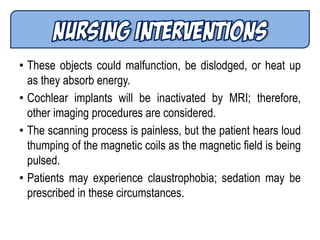
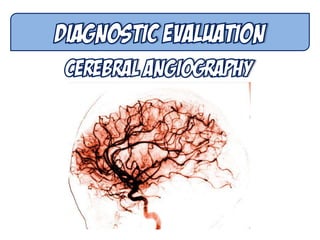
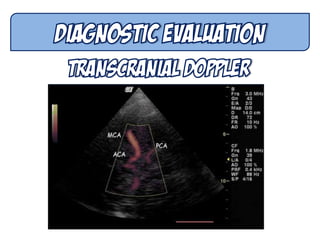
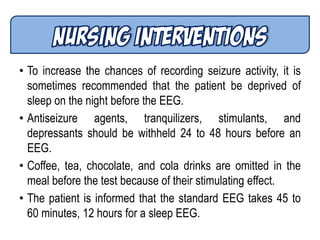
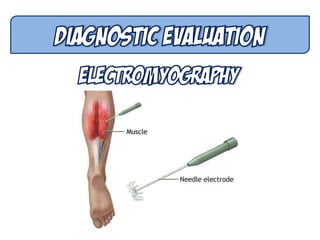
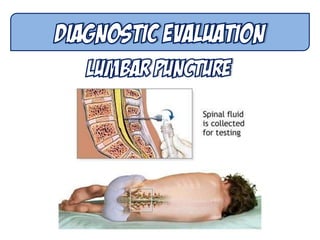
This document provides information on neurologic assessment. It begins by outlining the learning objectives which focus on describing the structure and function of the central and peripheral nervous systems, differentiating between pathologic changes that affect motor and sensory function, and comparing the sympathetic and parasympathetic nervous systems. It then provides detailed descriptions of the assessment of mental status, cranial nerves, motor function, sensation, and diagnostic tests for neurologic disorders. The assessments are aimed at identifying neurologic dysfunction.