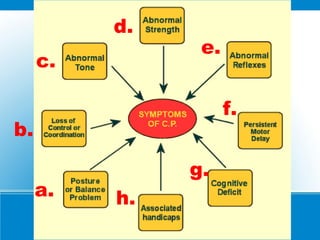
This document provides information about cerebral palsy, including:
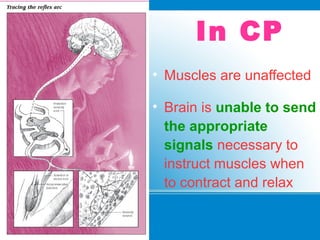
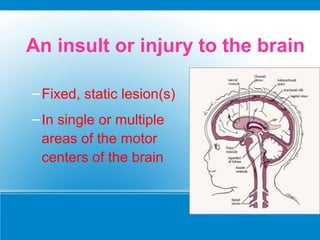
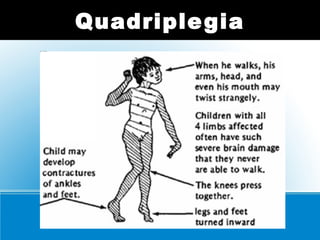
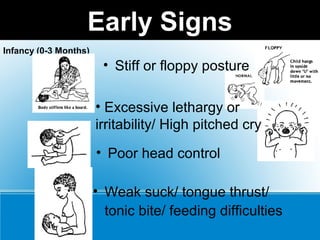
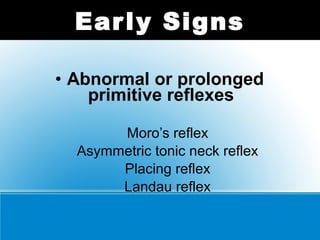
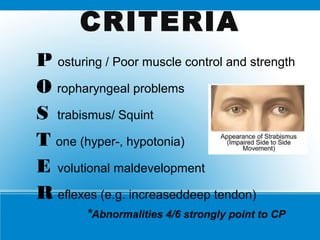
(1) It is a motor function disorder caused by permanent brain damage present at birth or shortly after.
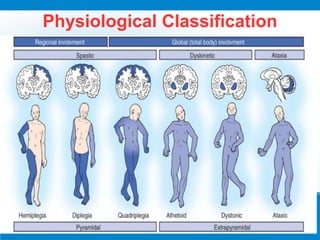
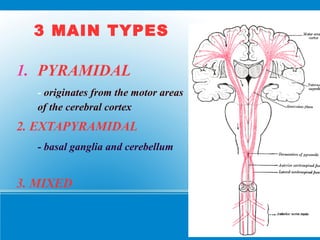
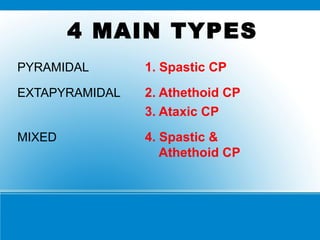
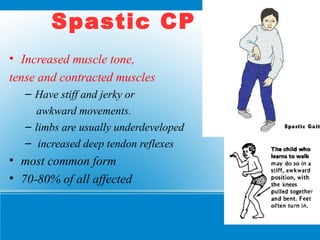
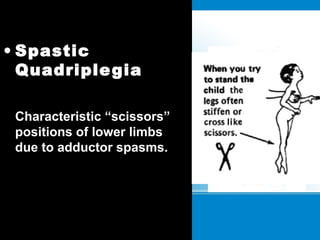
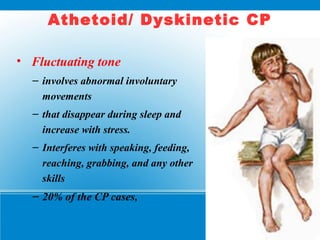
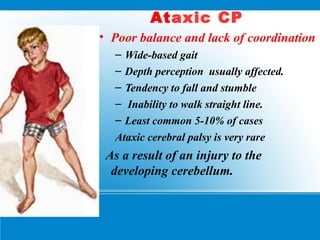
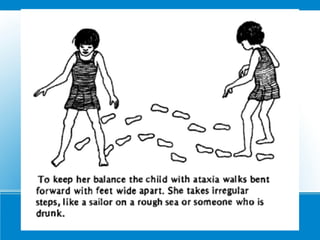
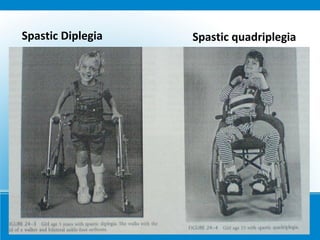
(2) The most common types are spastic cerebral palsy (stiff muscles) and athetoid cerebral palsy (uncontrolled movements).
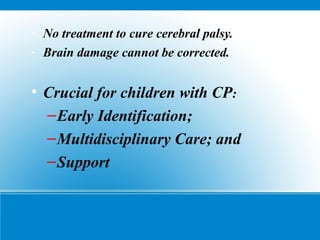
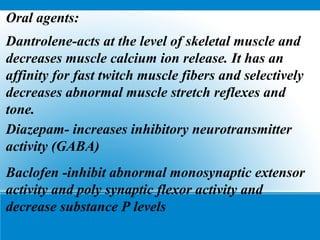
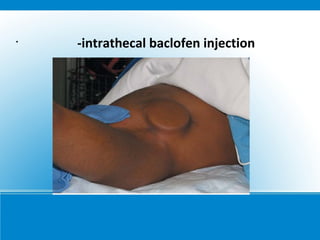
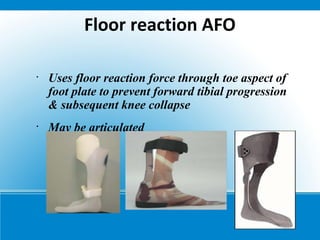
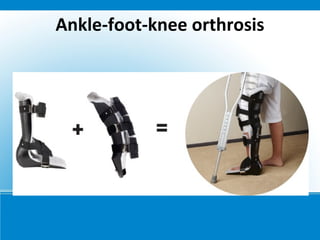
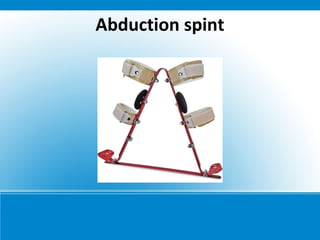
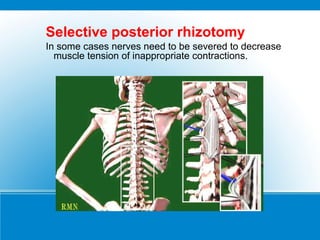
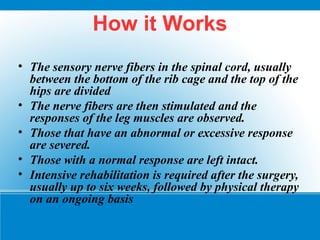
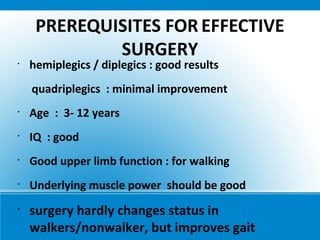
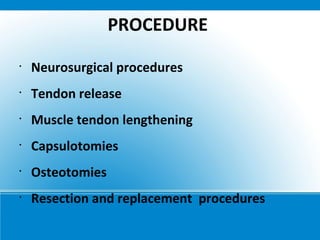
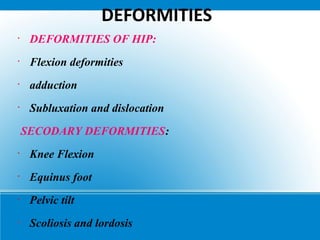
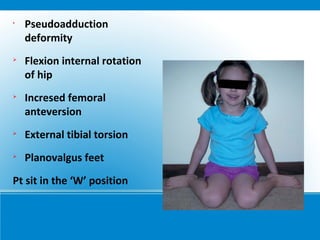
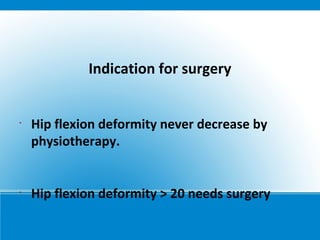
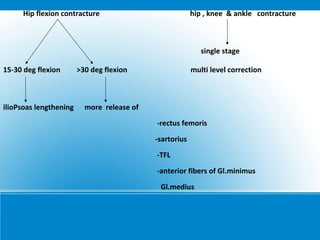
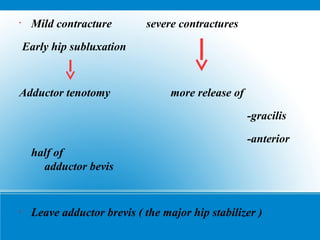
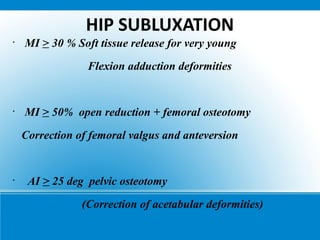
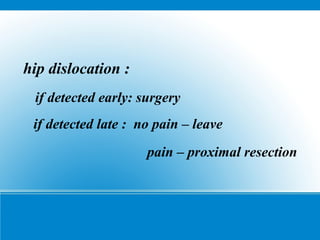
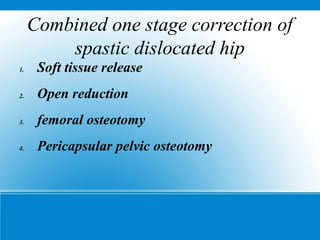
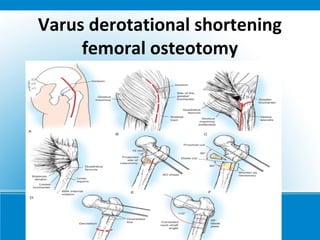
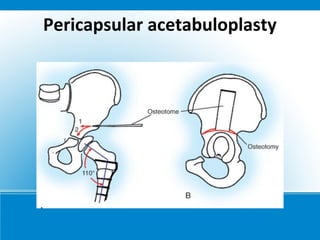
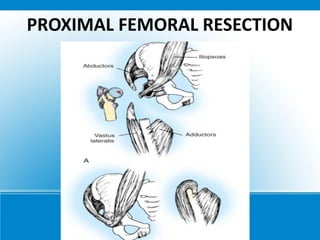
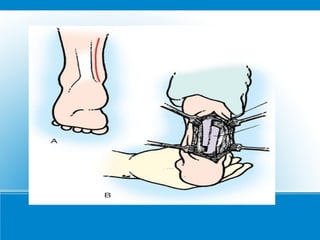
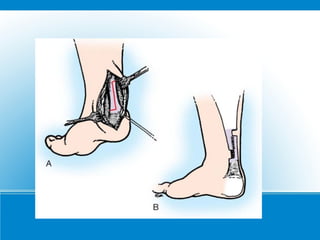
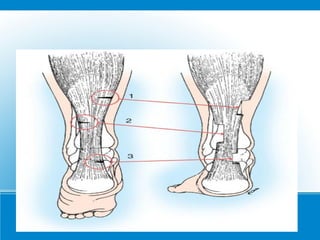
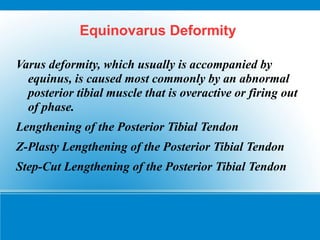
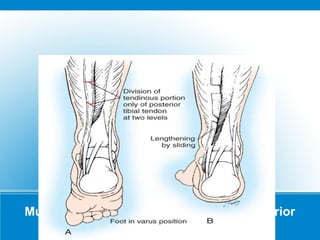
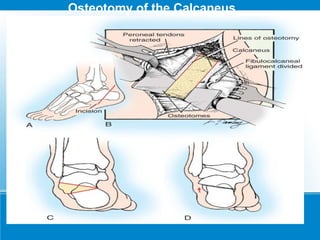
(3) Treatment aims to improve symptoms through physical therapy, bracing, medication, botulinum toxin injections, and sometimes surgery. The goal is improving quality of life and function rather than curing the underlying brain damage.