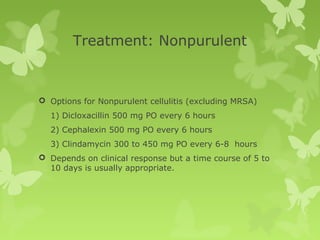
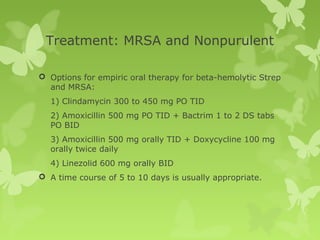
This document discusses cellulitis, including its definition, diagnosis, microbiology, and treatment approaches. It provides guidelines for treating non-purulent versus purulent cellulitis, and recommendations for oral versus intravenous antibiotics. Hospitalization is warranted for extensive or systemic infections, including the case presented of a patient with a large, draining leg wound requiring IV vancomycin.