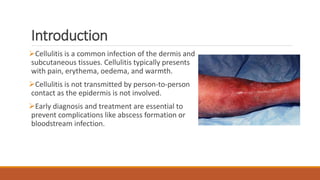
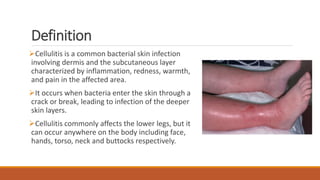
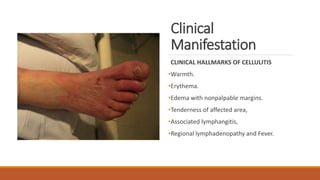
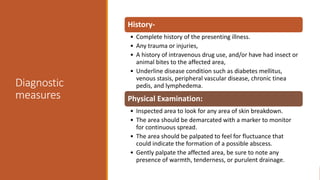
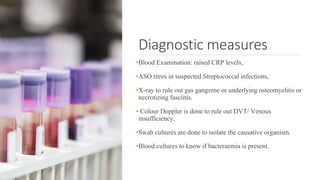
Cellulitis is a common bacterial skin infection that affects the dermis and subcutaneous layers, characterized by pain, swelling, warmth, and redness. It is crucial to diagnose and treat early to prevent complications like abscess formation or bacteremia, and management often includes antibiotics and supportive care. Risk factors include skin injuries, diabetes, obesity, and immunocompromised states, and prevention emphasizes good hygiene and care of skin abrasions.