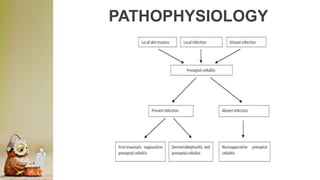
Cellulitis is a bacterial skin infection of the dermis and subcutaneous fat, most commonly caused by Staphylococcus or Streptococcus bacteria. It has an incidence rate of 24.6 per 1,000 person-years and most often affects the lower extremities. Risk factors include local skin trauma, pre-existing skin infections, and immunosuppression. Mild cases are treated with oral antibiotics while more severe cases require intravenous antibiotics and hospitalization. Complications can include blood infections, bone infections, and in rare cases, tissue death.