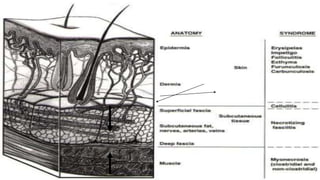
1. The document discusses skin and soft tissue infections (SSTIs) such as cellulitis and abscesses.
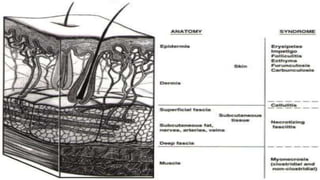
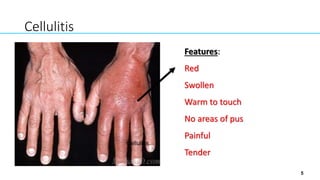
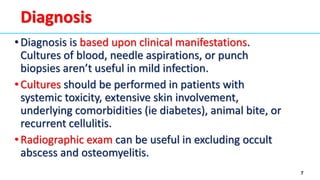
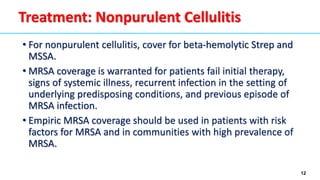
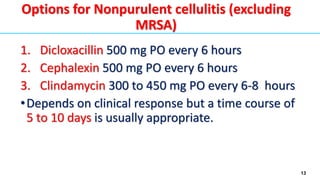
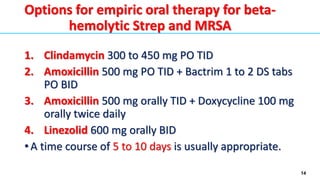
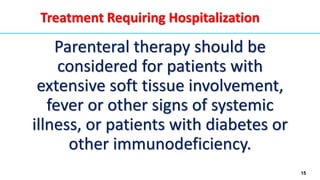
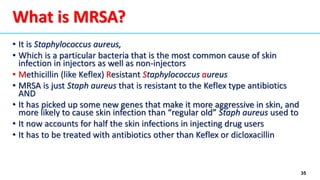
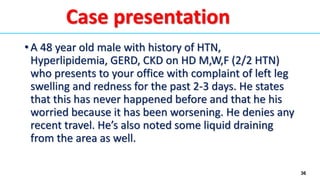
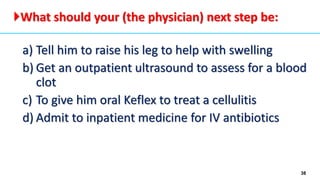
2. Cellulitis manifests as erythema, edema, and warmth. Diagnosis is based on clinical examination. Common causes are Strep and Staph bacteria.
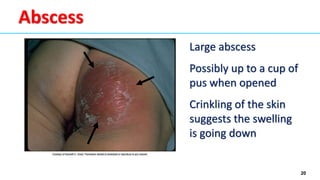
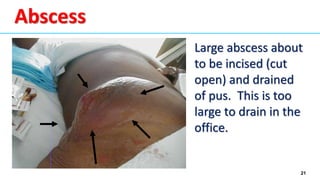
3. Abscesses form when pus develops within the site of cellulitis. Abscesses should be drained to treat the infection.
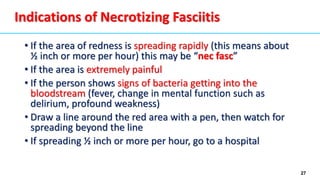
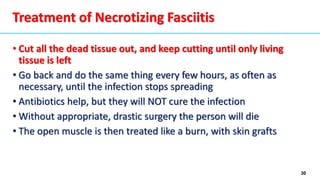
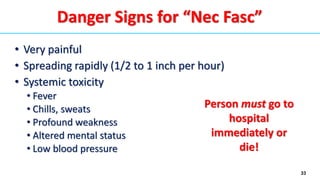
4. Necrotizing fasciitis is a severe infection where bacteria rapidly spread between fat and muscle tissues, causing tissue death. Immediate surgery is needed to remove dead tissue or the infection will be fatal.