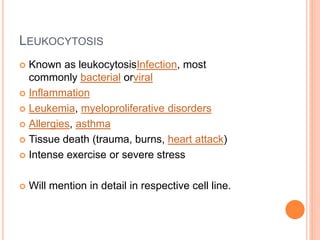
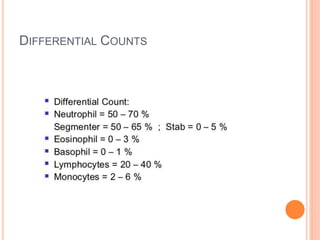
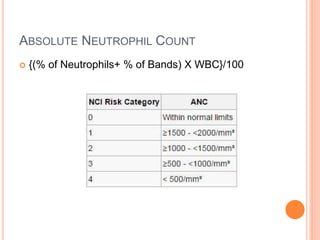
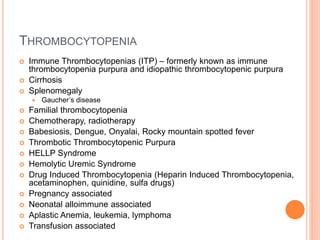
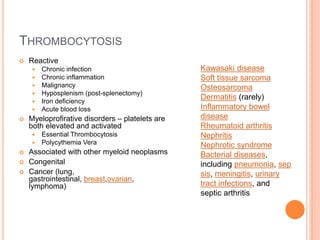
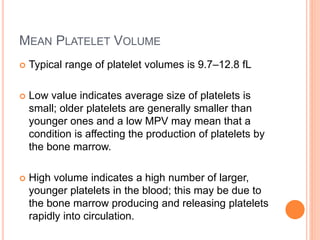
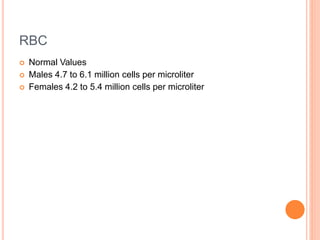
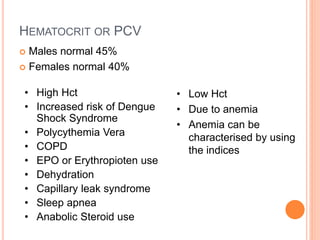
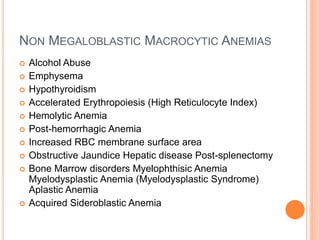
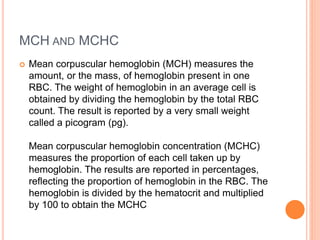
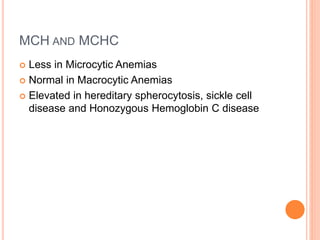
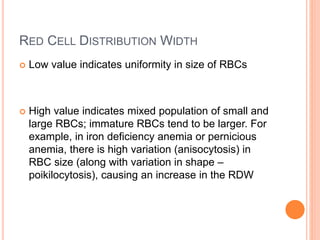
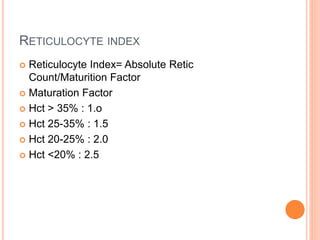
The document provides a comprehensive interpretation of complete blood count (CBC) parameters, including red blood cells (RBC), white blood cells (WBC), and platelets, along with their normal ranges and implications of deviations. It outlines the conditions associated with low and high counts for each component, such as anemia, leukopenia, and thrombocytopenia, while also discussing the significance of various indices related to blood counts. Overall, the document serves as a guide for clinical assessment and diagnosis based on CBC results.


![DRUGS CAUSING LEUKOPENIA
LOADS!!!
Clozapine, buproprion, valproic acid, minocycline,
lamotrigine.
Immunosuppressive drugs, such
as sirolimus, mycophenolate
mofetil, tacrolimus, cyclosporine, Leflunomide
(Arava) and TNF inhibitors.[2] Interferonsused to
treat multiple sclerosis, such as Rebif, Avonex,
and Betaseron, can also cause leukopenia.
Chemotherapeutic drugs.
Lots of others.](https://image.slidesharecdn.com/cbc-150106153749-conversion-gate02/85/Complete-Blood-Count-Interpretations-22-320.jpg)