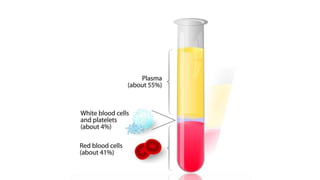
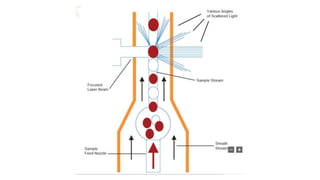
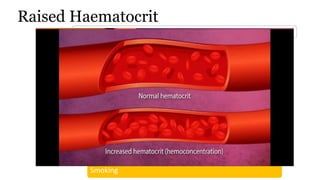
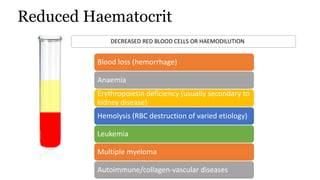
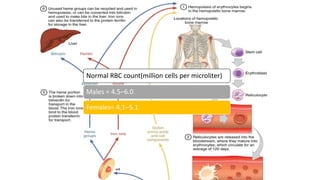
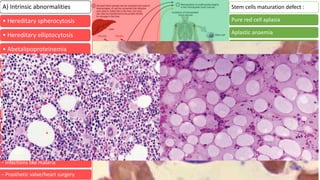
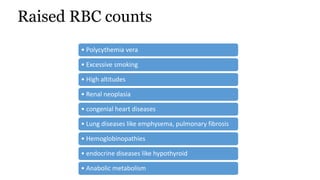
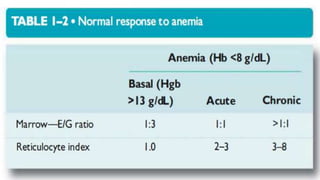
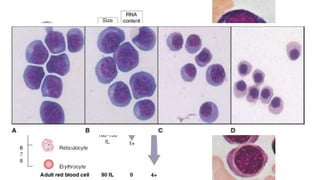
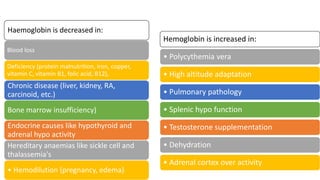
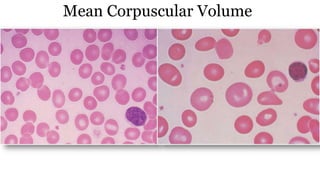
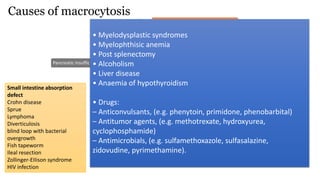
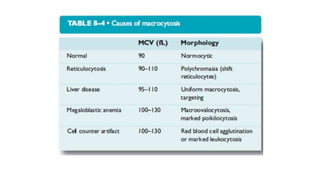
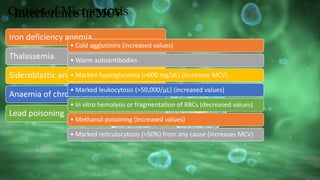
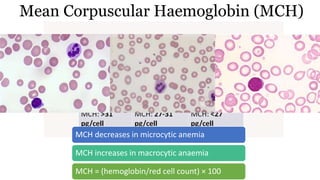
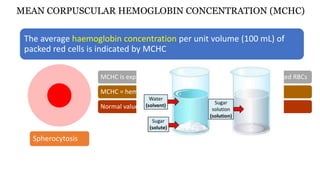
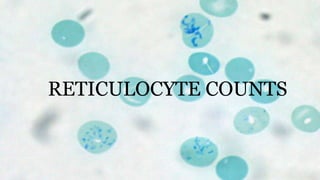
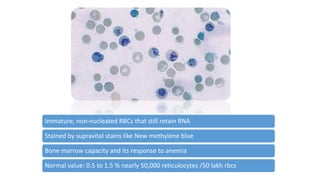
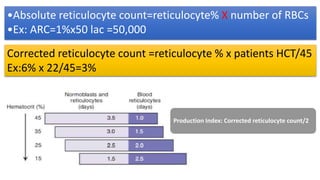
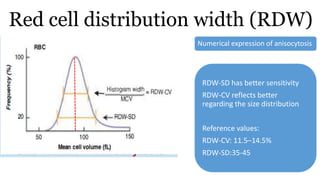
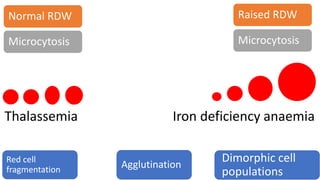
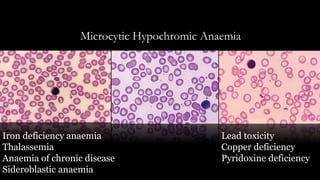
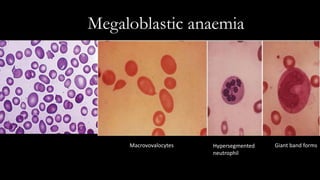
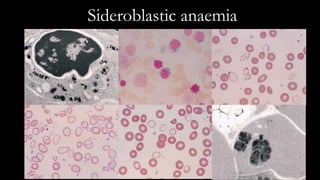
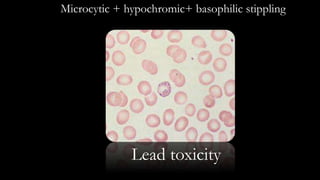
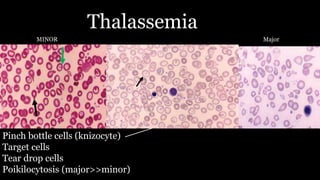
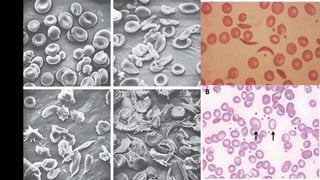
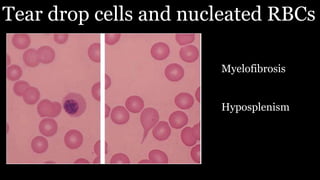
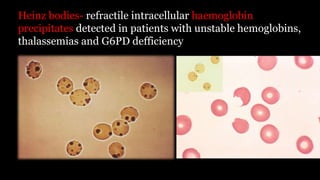
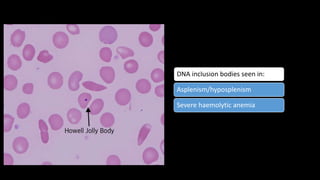
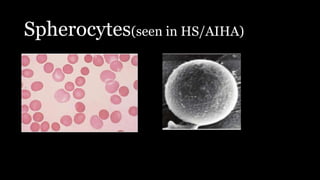
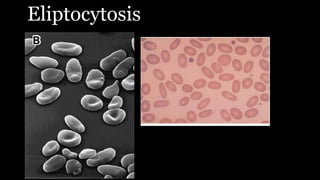
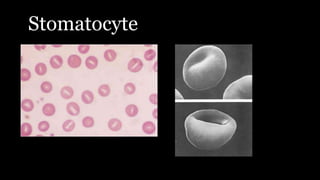
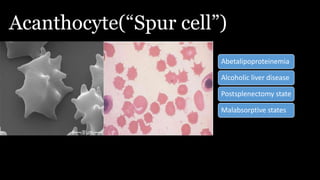
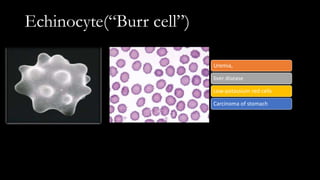
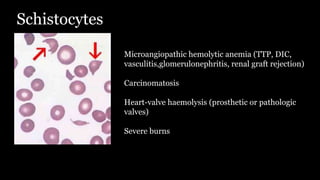
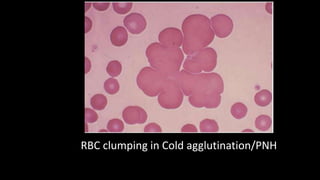
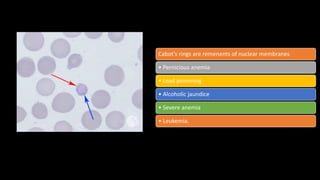
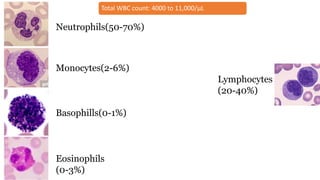
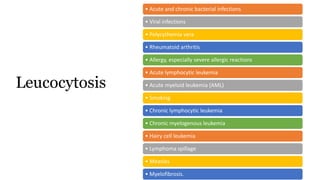
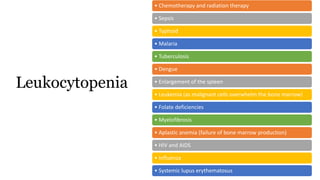
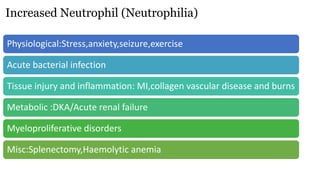
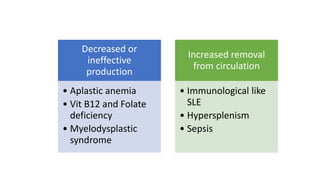
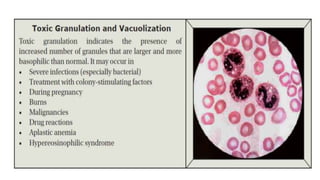
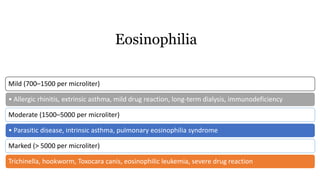
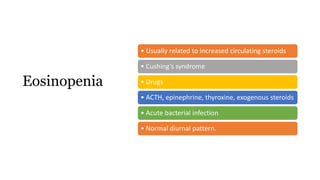
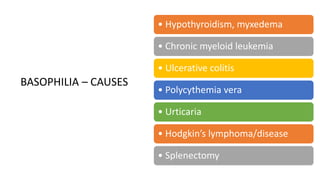
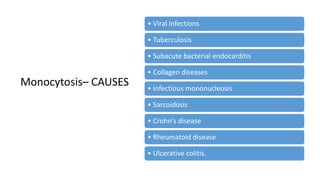
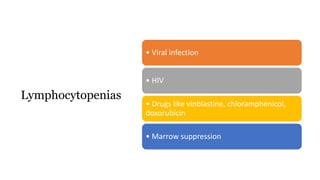
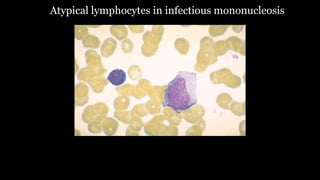
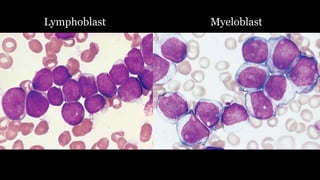
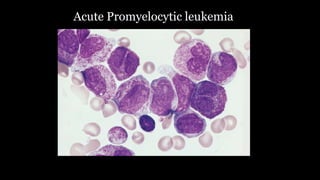
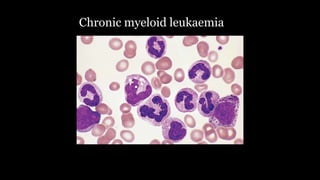
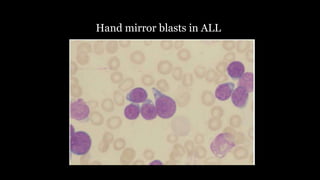
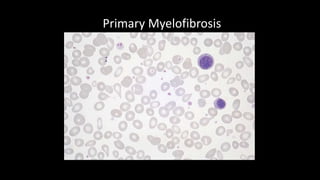
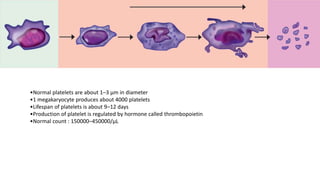
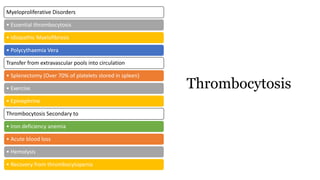
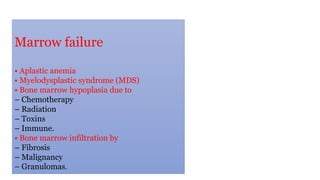
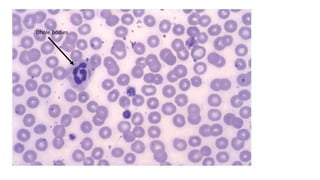
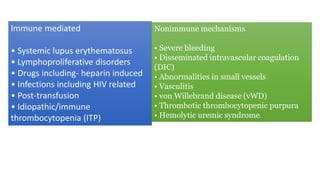
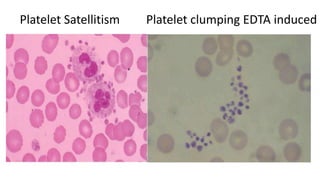
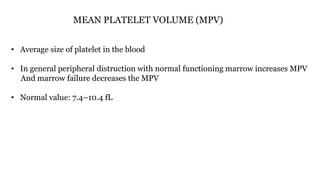
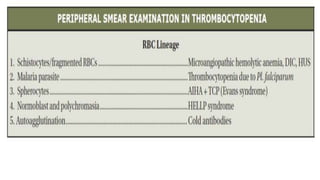
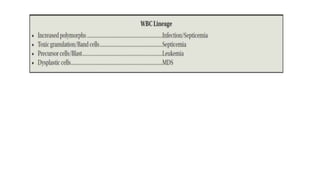
The document provides an extensive overview of complete blood count parameters, including hematocrit, hemoglobin, white blood cells, and platelet counts, along with their normal ranges and various conditions leading to abnormalities. It discusses factors causing increased or decreased blood components, such as anemia, leukocytosis, and thrombocytopenia, as well as the clinical implications of these variations. Additionally, it details specific morphologies and their associations with different pathologies, emphasizing the significance of proper analysis in diagnosing hematological disorders.