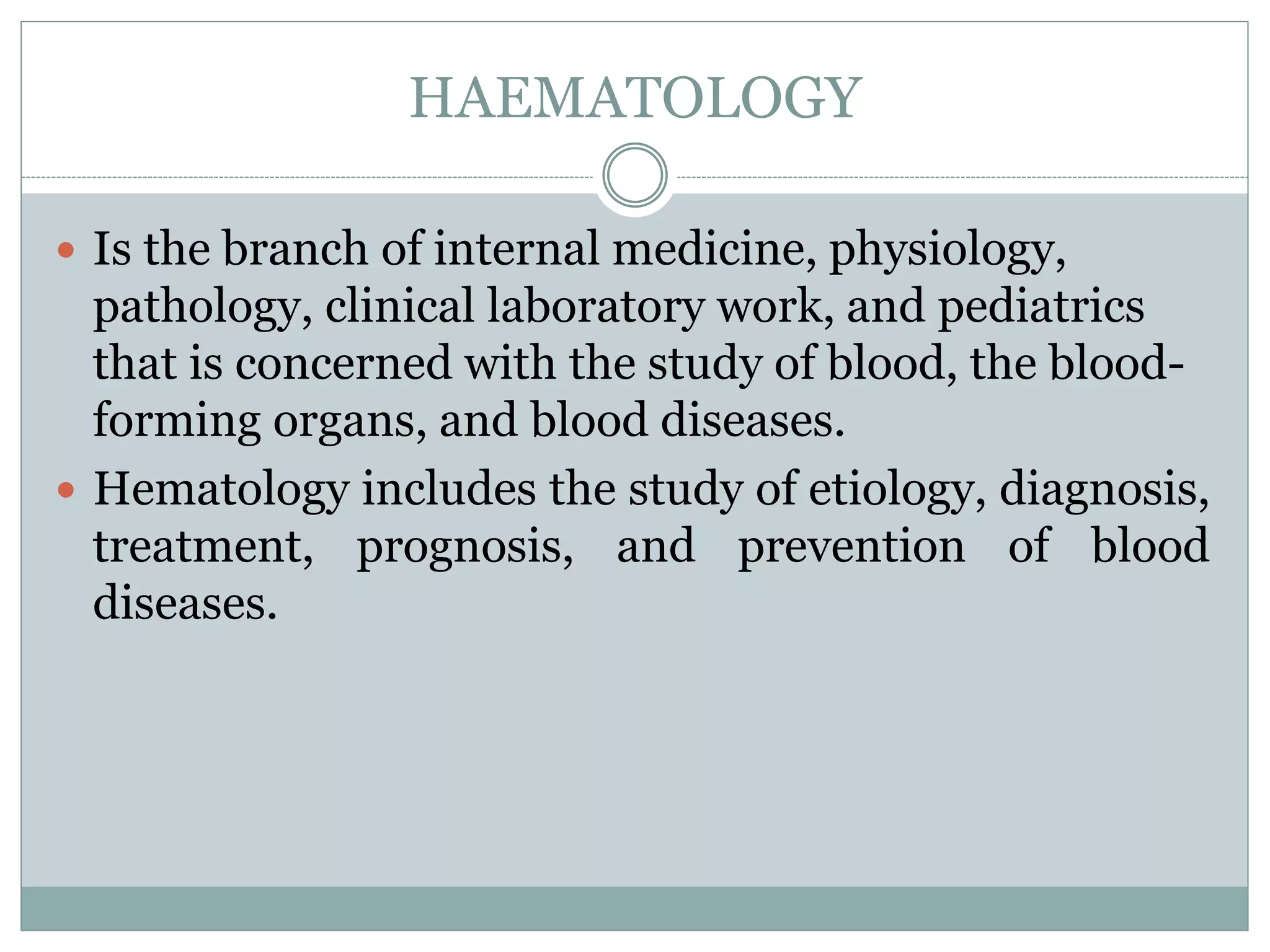
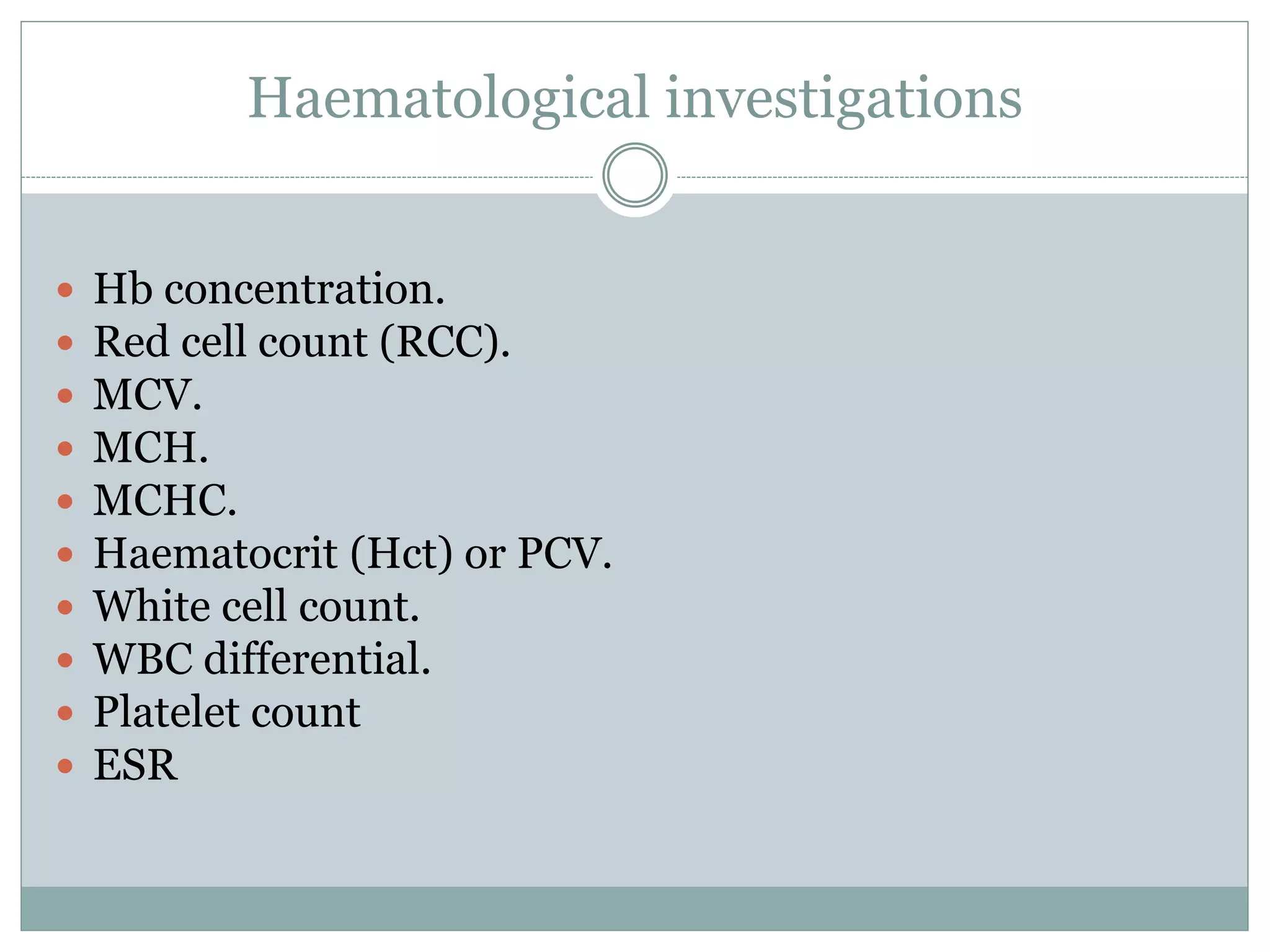
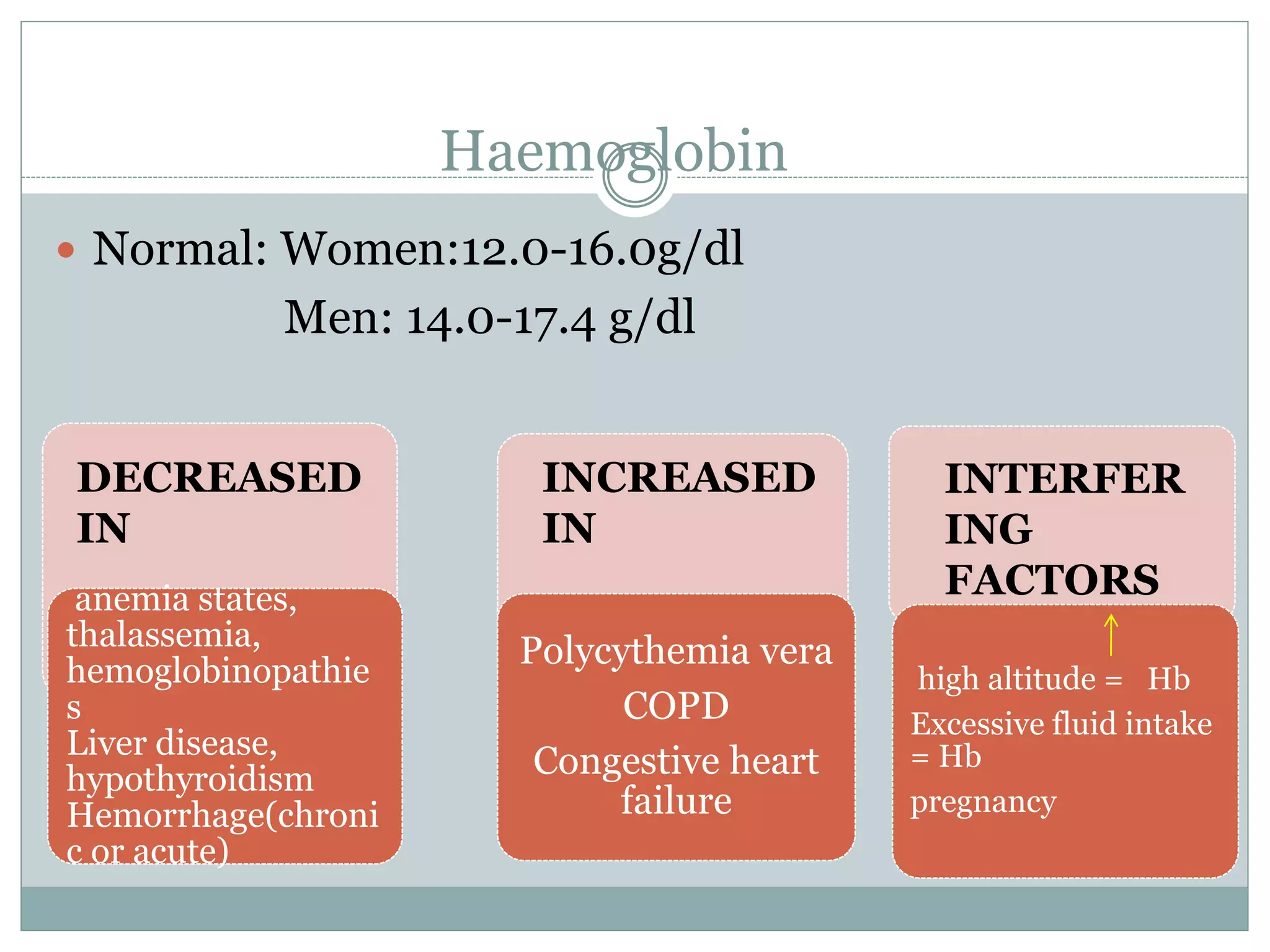
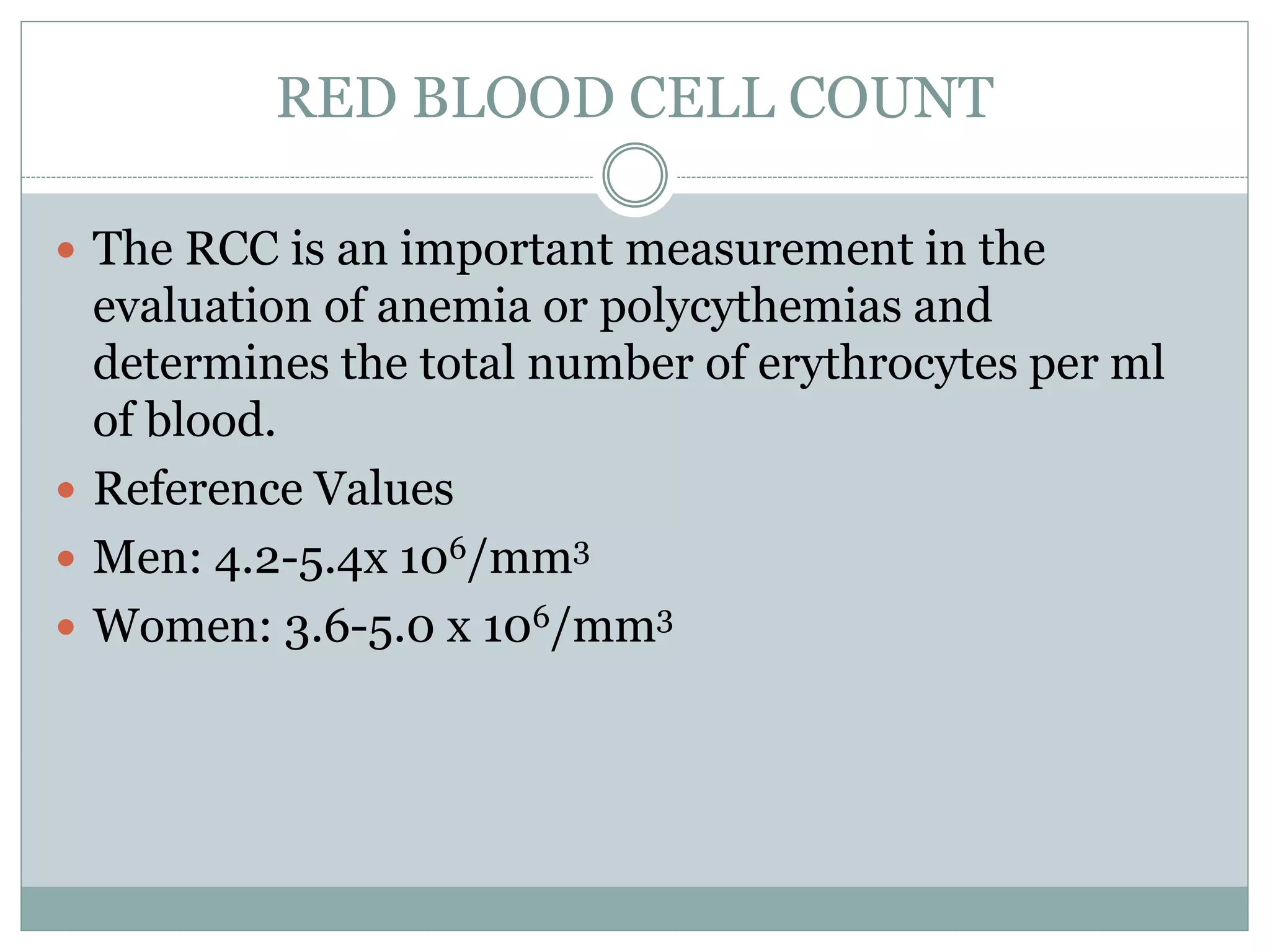
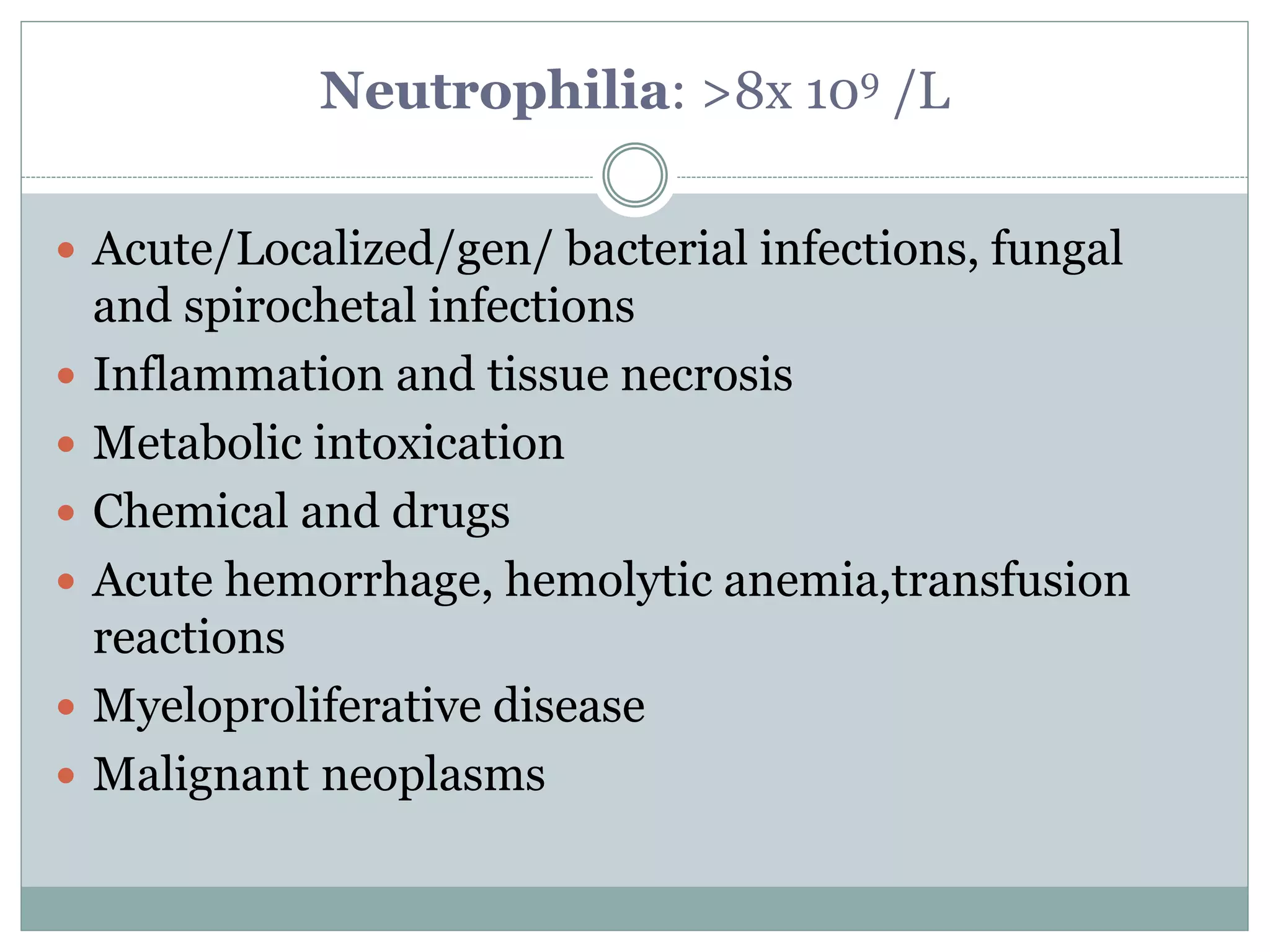
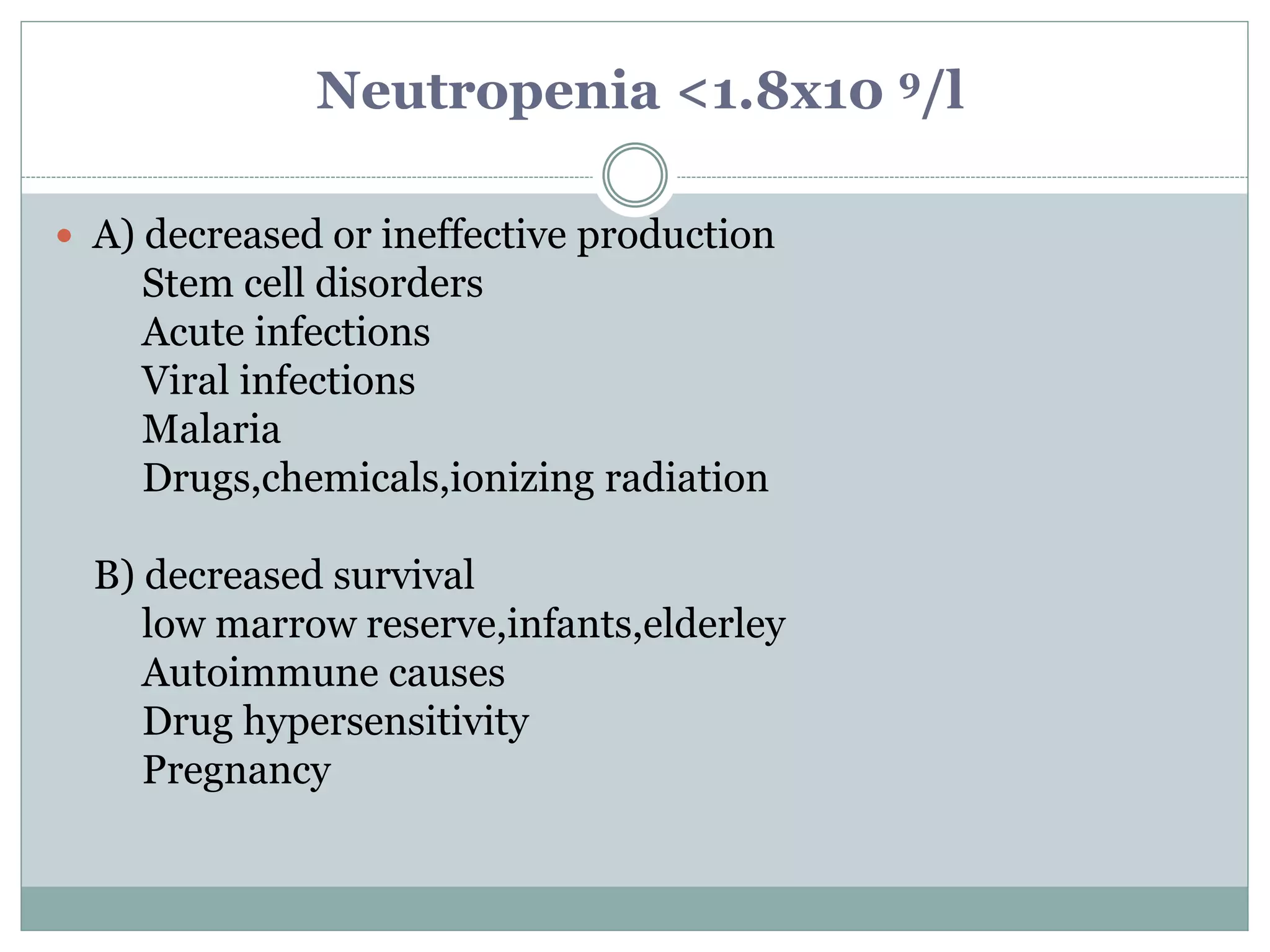
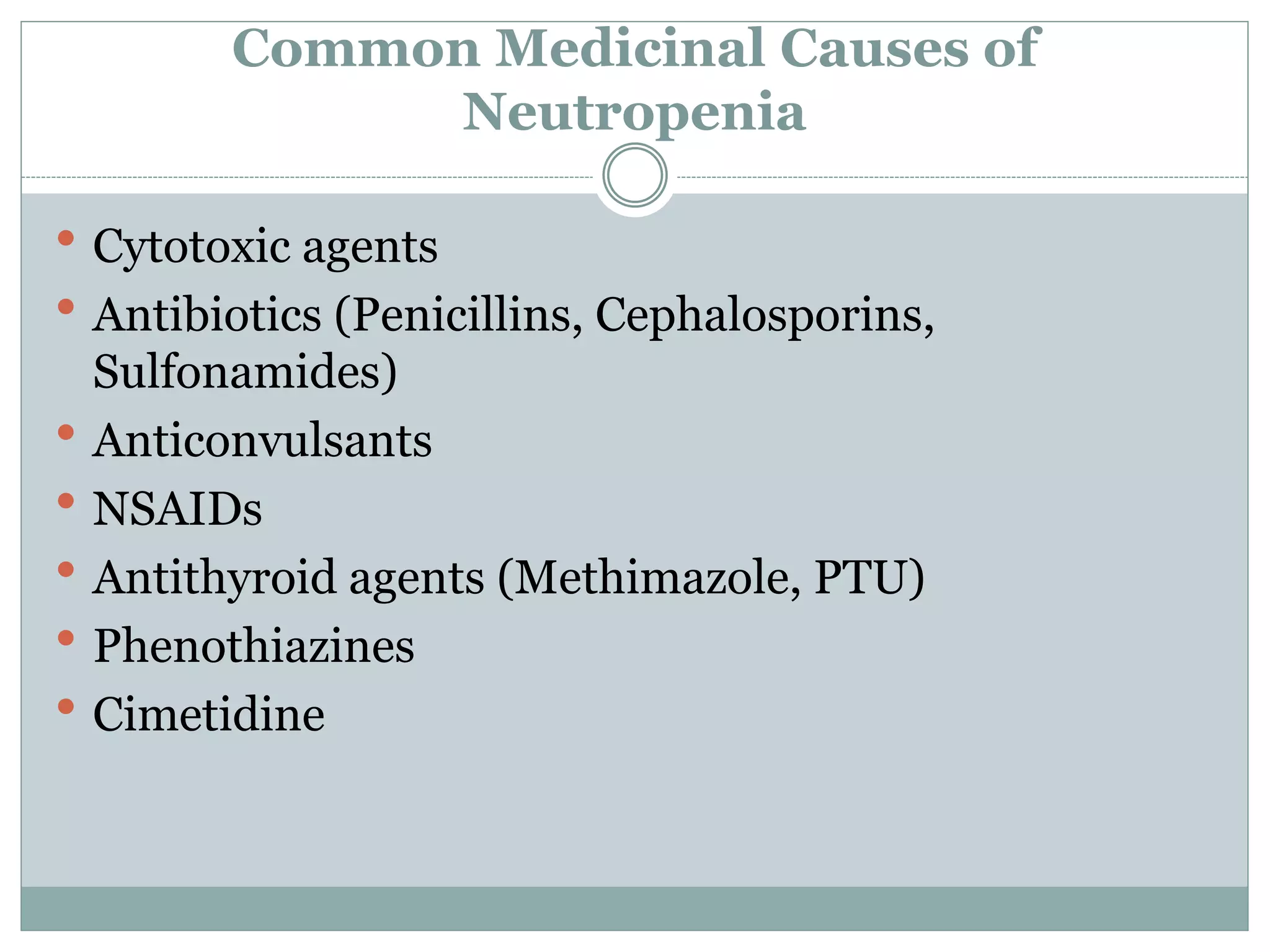
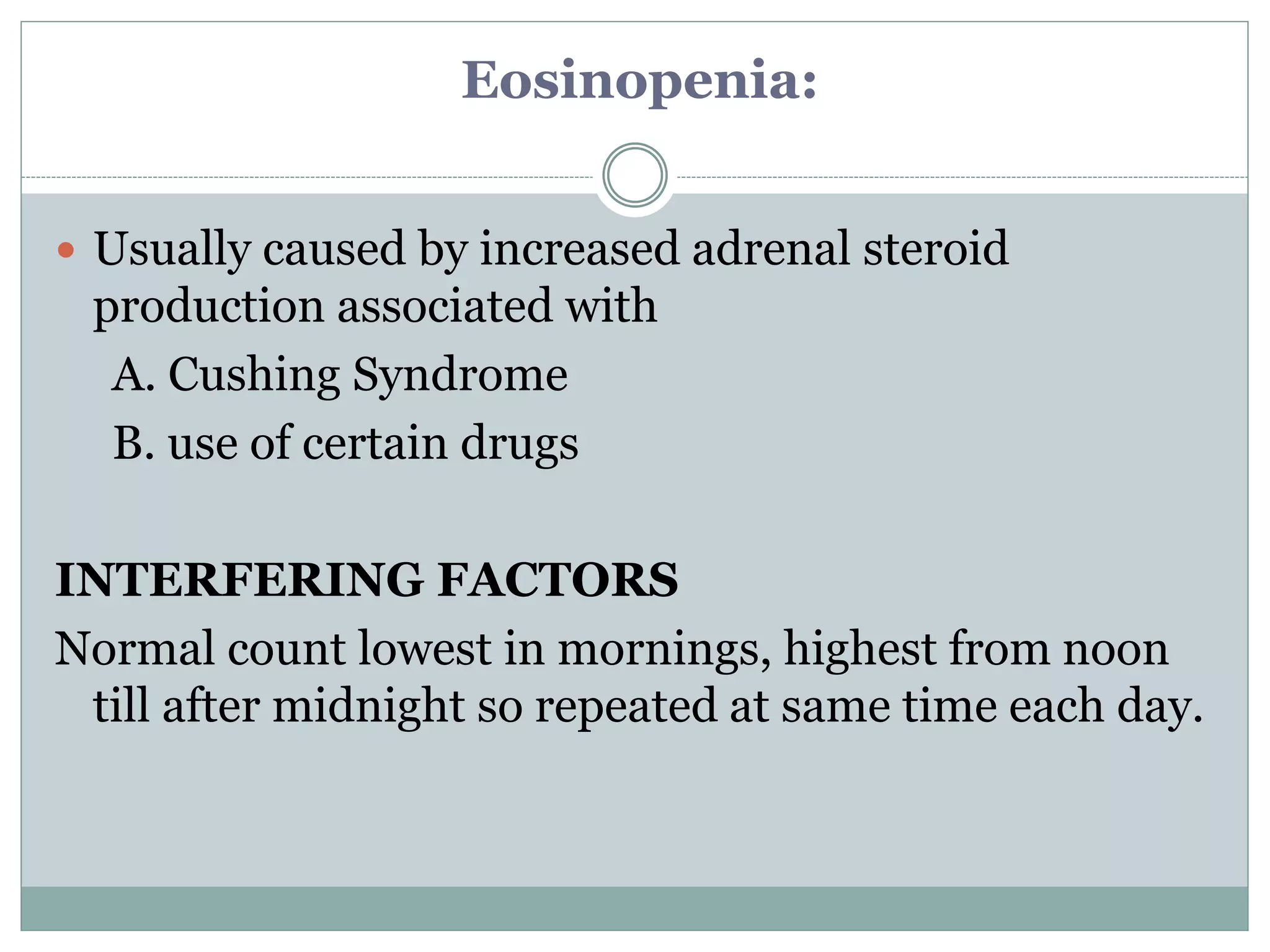
This document discusses various laboratory investigations used in oral and maxillofacial surgery (OMFS). It describes hematological tests including complete blood count, red blood cell indices, platelet count, and bleeding time. It outlines normal ranges and clinical implications of increased or decreased results for hematological parameters. These laboratory tests provide important information to establish medical diagnoses and guide patient management in OMFS.






























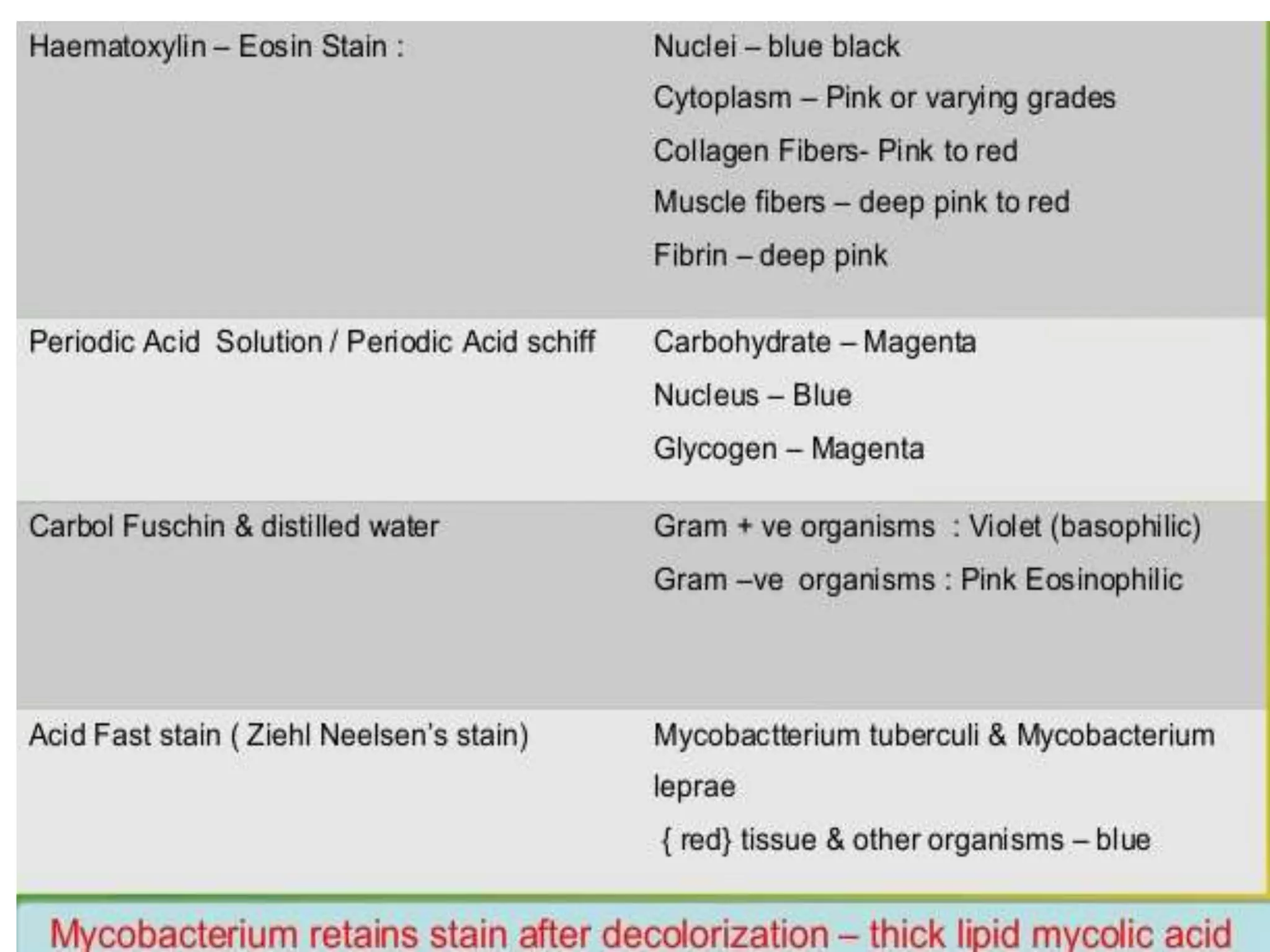



![Rh Typing
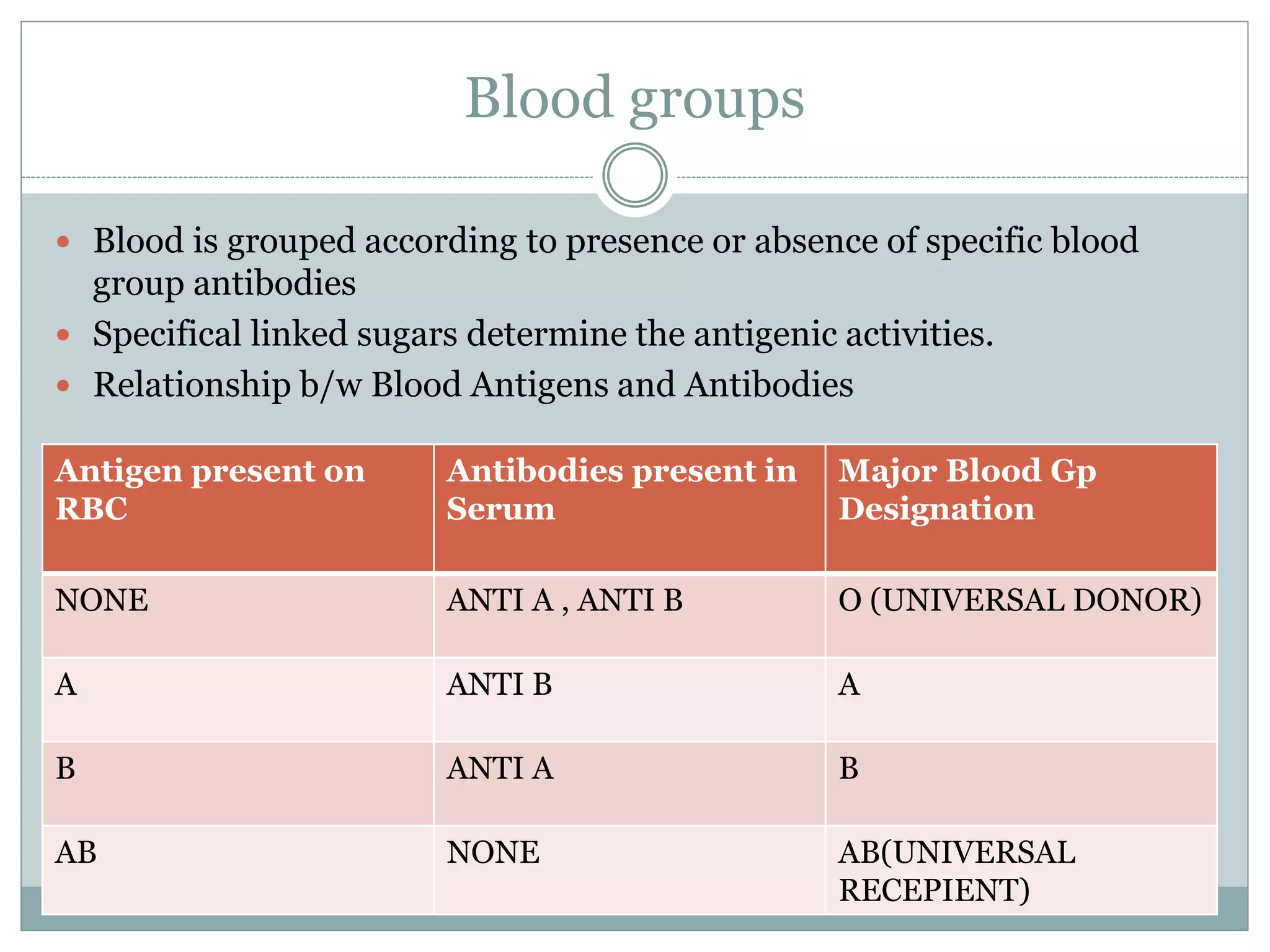
Human blood is classified as Rh +ve or -ve
Relates to presence or absence of D antigen on the RBC
membrane.(now called the Rh1[D] antigen
Rh –ve individuals may develop antibodies against Rh
positive antigens if they are challenged through a transfusion
of Rh +ve blood or through a fetomaternal bleed from an Rh
+ve fetus
Rh typing must be done because:
Rh +ve blood administered to Rh –ve person may sensitize
the person to form anti-D(Rh1)
Rh +ve blood to person having serum anti-D. ~Fatal
Rh –ve pregnant women:RhIG dose antepartum at 28 weeks
of gestation and a postpartum inj. Shortly after delivery of an
Rh +ve infant](https://image.slidesharecdn.com/labinvestigations-ih-160522072506/75/Lab-investigations-in-OMFS-ih-92-2048.jpg)

