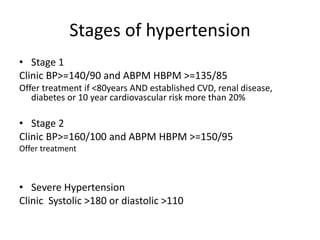
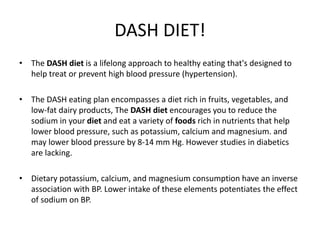
This document summarizes guidelines for the treatment and management of hypertension. It discusses stages of hypertension and treatment thresholds. Lifestyle modifications like following the DASH diet, reducing sodium intake, weight loss, and exercise are recommended first line approaches. If goals are not met with lifestyle changes alone, pharmacologic therapy with diuretics, ACE inhibitors, ARBs, calcium channel blockers, and beta blockers is recommended. Specific considerations and guidelines are provided for managing hypertension in special populations like those with diabetes, pregnancy, the elderly, and black patients.






![Management of Hypertensive
Emergencies
• Hypertensive emergencies are characterized by severe elevations in BP
(>180/120 mm Hg) associated with acute end-organ damage
• Examples include hypertensive encephalopathy, intracerebral
hemorrhage, acute myocardial infarction, acute left ventricular failure
with pulmonary edema, aortic dissection, unstable angina pectoris,
eclampsia, [2] or posterior reversible encephalopathy syndrome (PRES) (a
condition characterized by headache, altered mental status, visual
disturbances, and seizures)](https://image.slidesharecdn.com/bparticle-discussion-180209094250/85/Blood-Pressure-Discussion-14-320.jpg)

![• Exceptions to the above recommendation include the following[2] :
• Patients with an ischemic stroke (currently, no clear evidence exists
for immediate antihypertensive treatment)
• Patients with aortic dissection (their systolic BP should be lowered
to < 100 mm Hg, if tolerated)
• Patients in whom BP is lowered to allow thrombolytic therapy (eg,
stroke patients)
• Avoid using short-acting nifedipine in the initial treatment of this
condition because of the risk of rapid, unpredictable hypotension
and the possibility of precipitating ischemic events.](https://image.slidesharecdn.com/bparticle-discussion-180209094250/85/Blood-Pressure-Discussion-16-320.jpg)
![• Women who have preexisting end-organ damage from chronic
hypertension or who have previously required multidrug therapy
for BP control should have a lower threshold for starting
antihypertensive medication (ie, >139/89 mm Hg) and a lower
target BP (< 140/90 mm Hg).
• Methyldopa is generally the preferred first-line agent because of its
safety profile.
• ]Other drugs labetalol, beta-blockers, and diuretics. Data are limited
regarding the use of clonidine and calcium antagonists in pregnant
women with chronic hypertension;
• however, angiotensin-converting enzyme (ACE) inhibitors and
angiotensin II receptor (ARB) antagonists should be avoided
because of the risk of fetal toxicity and death](https://image.slidesharecdn.com/bparticle-discussion-180209094250/85/Blood-Pressure-Discussion-18-320.jpg)