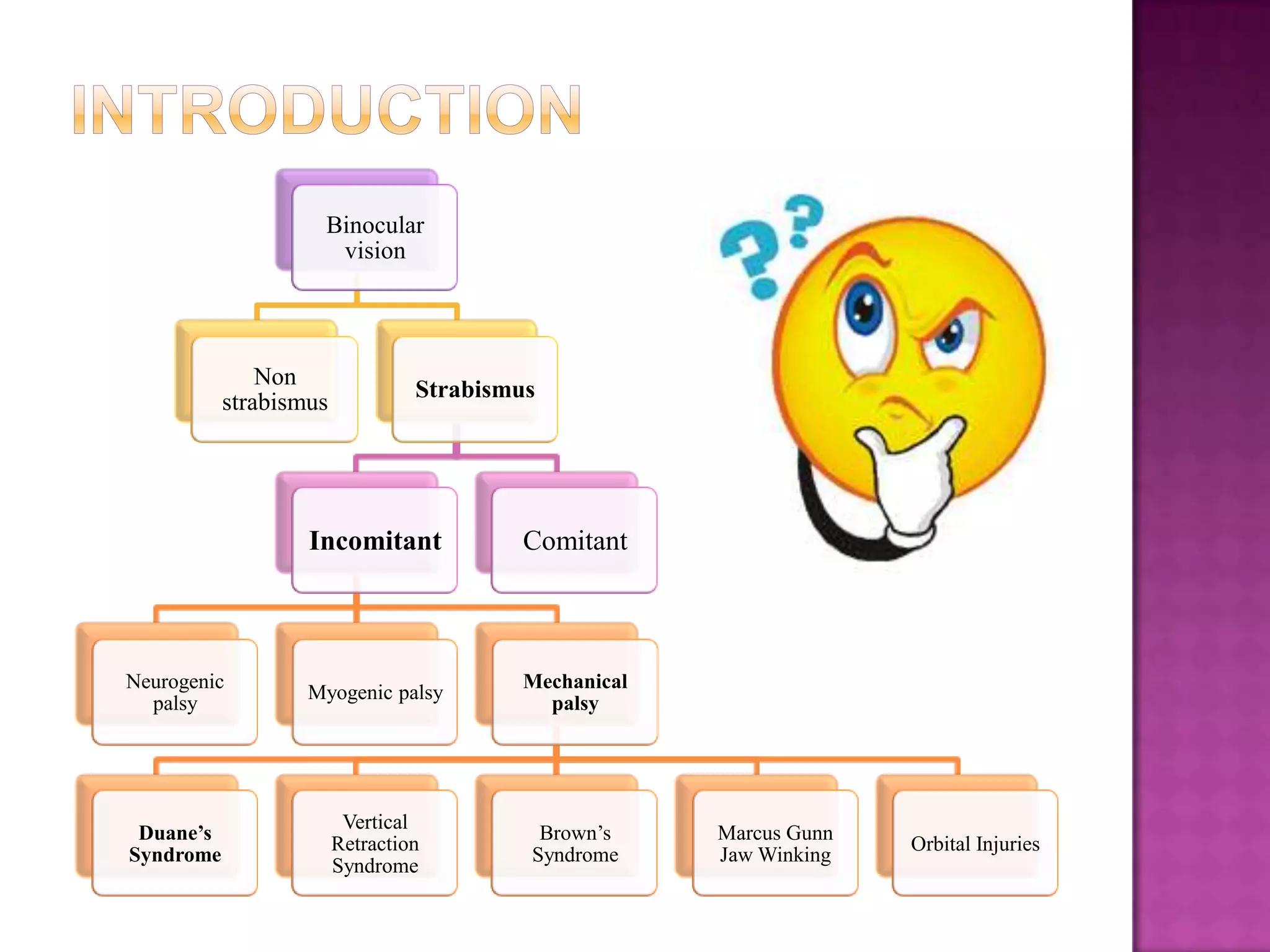
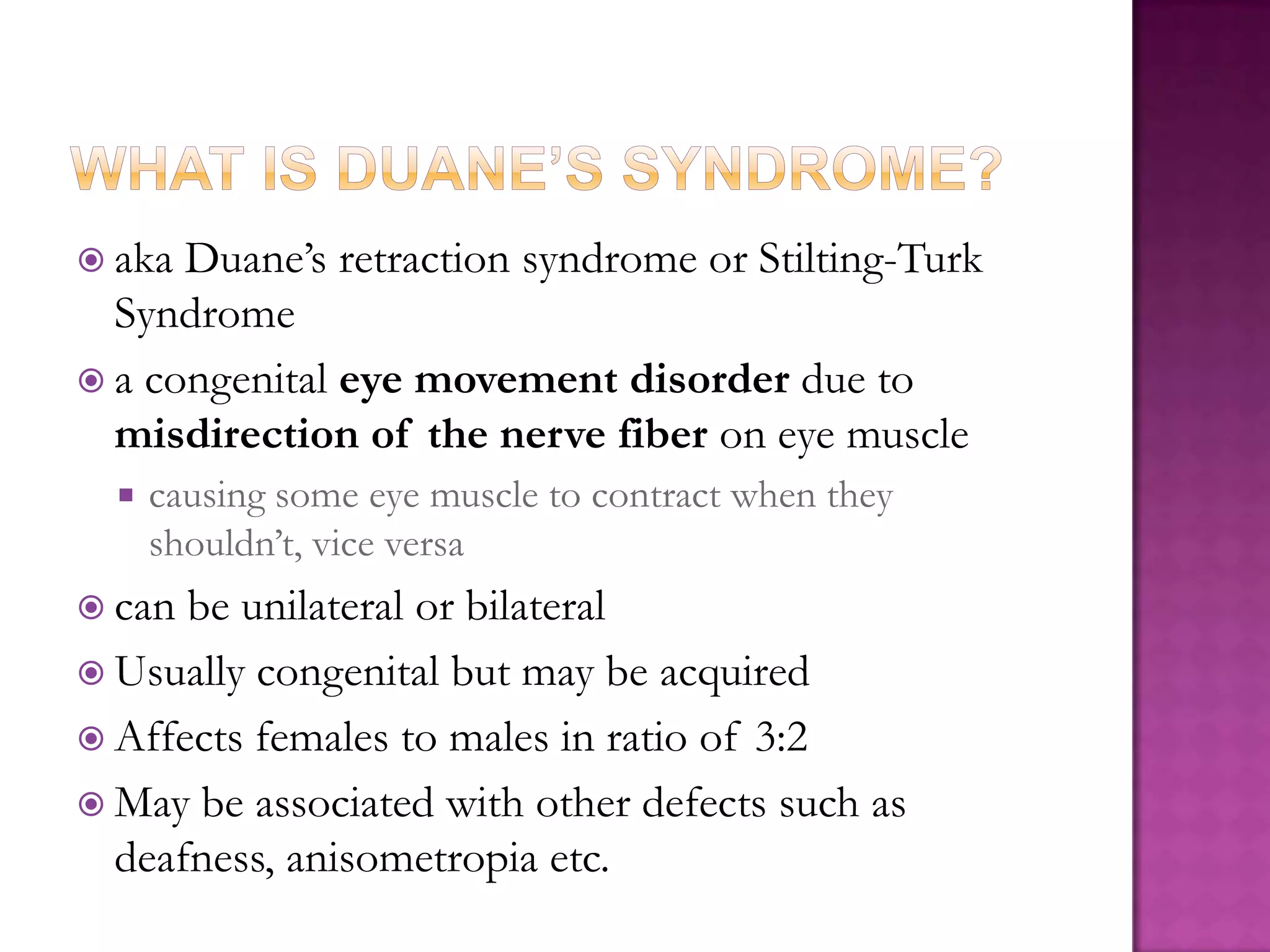
This document summarizes the key information about Duane's syndrome including:
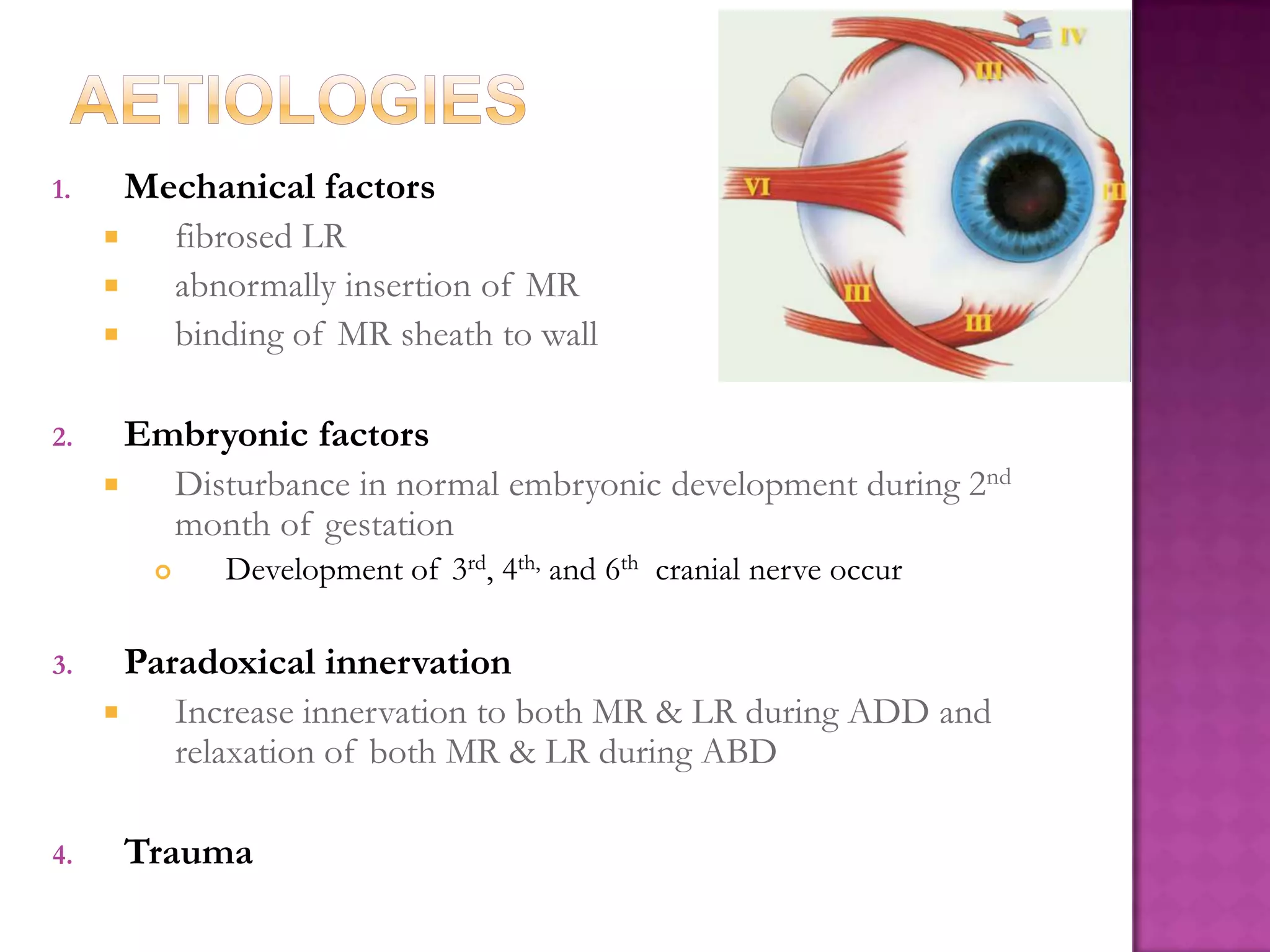
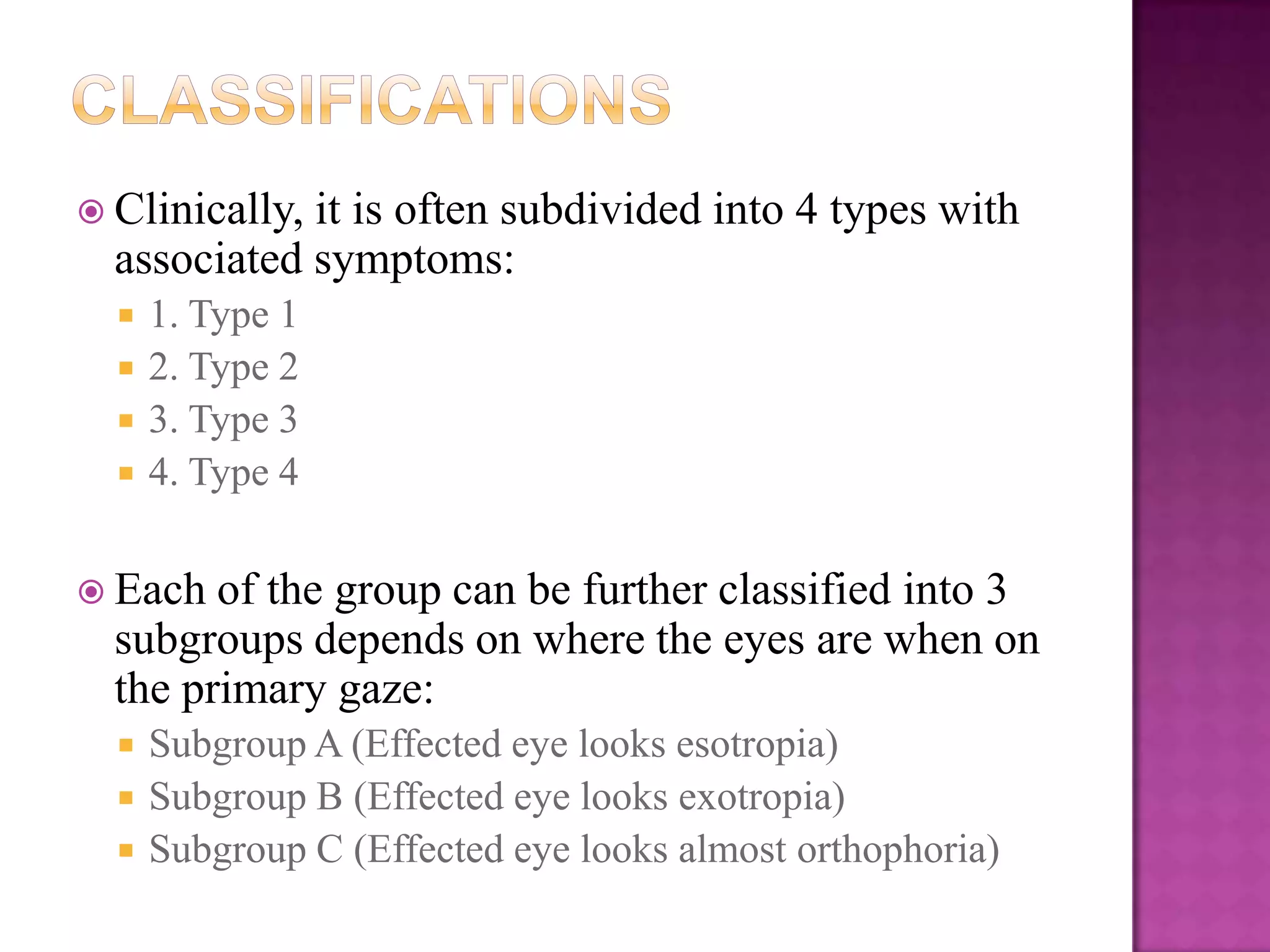
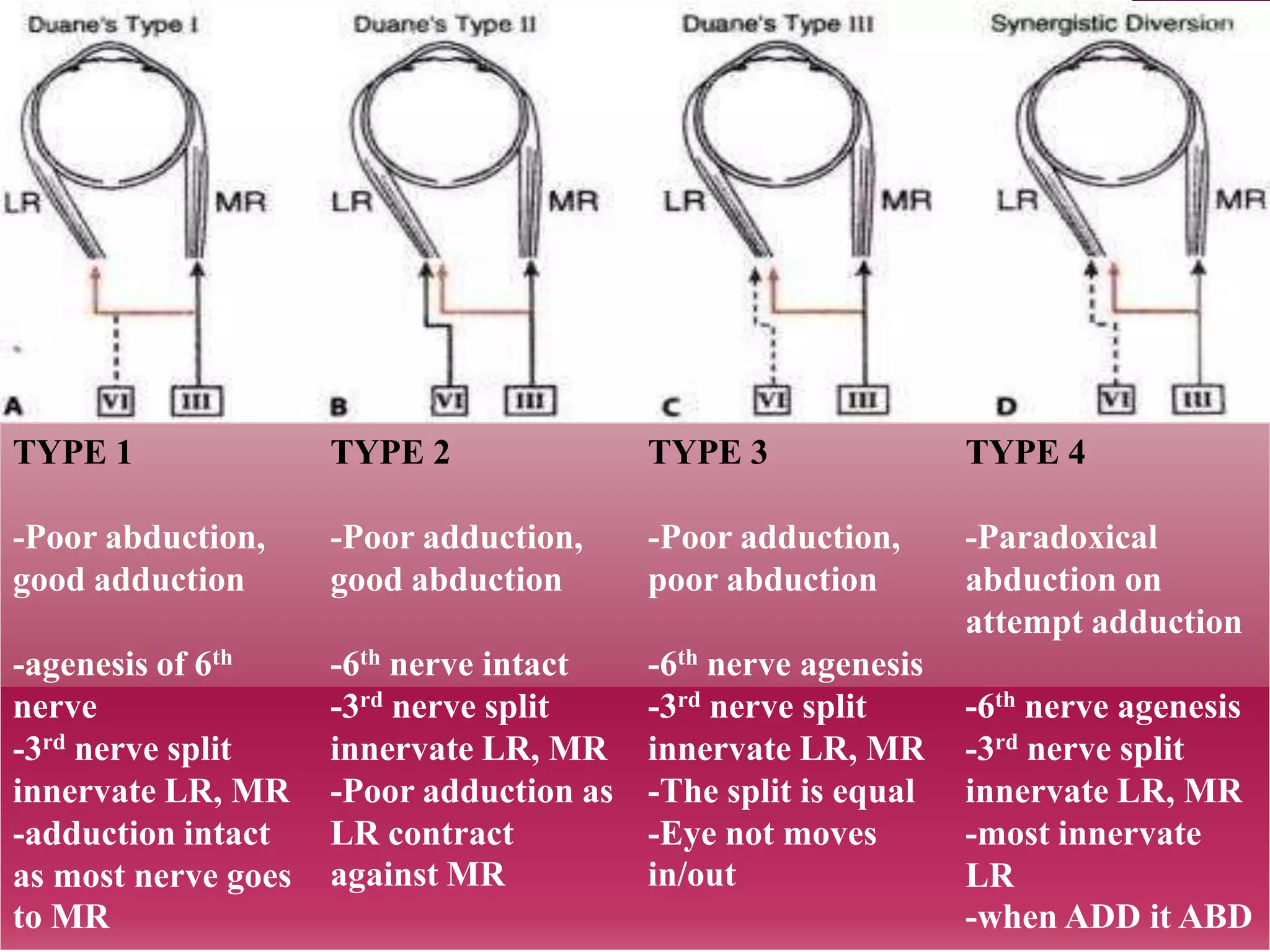
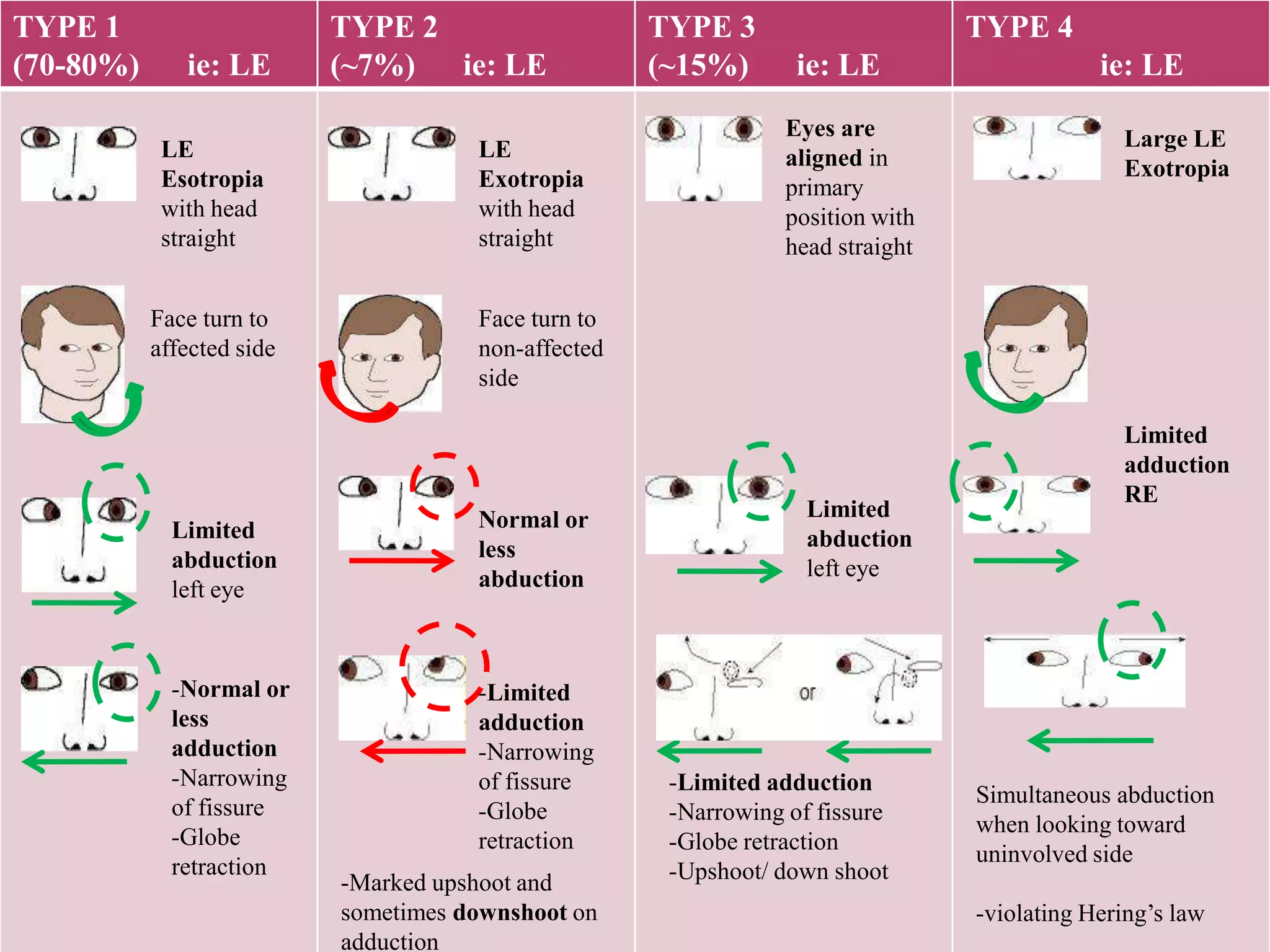
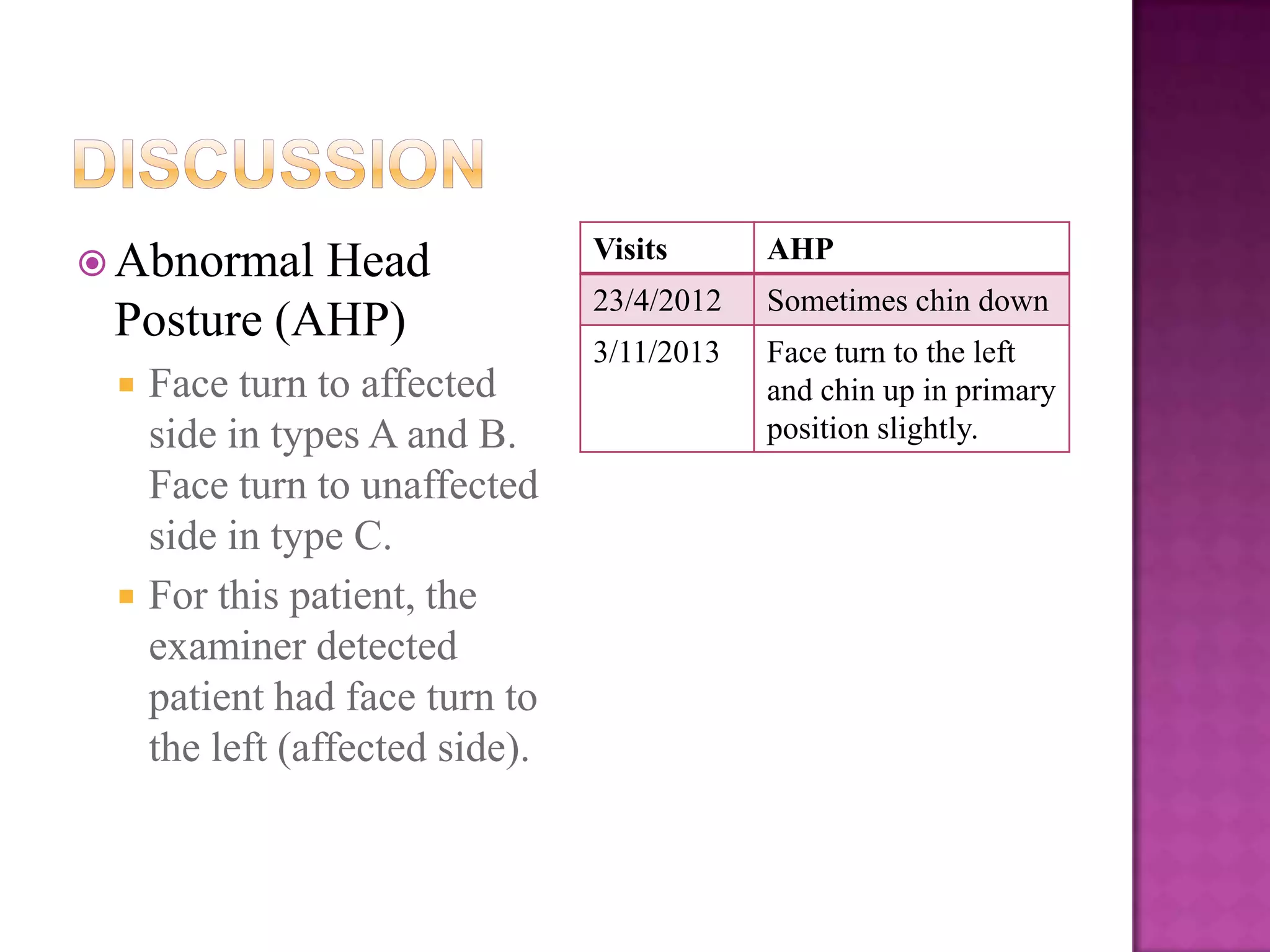
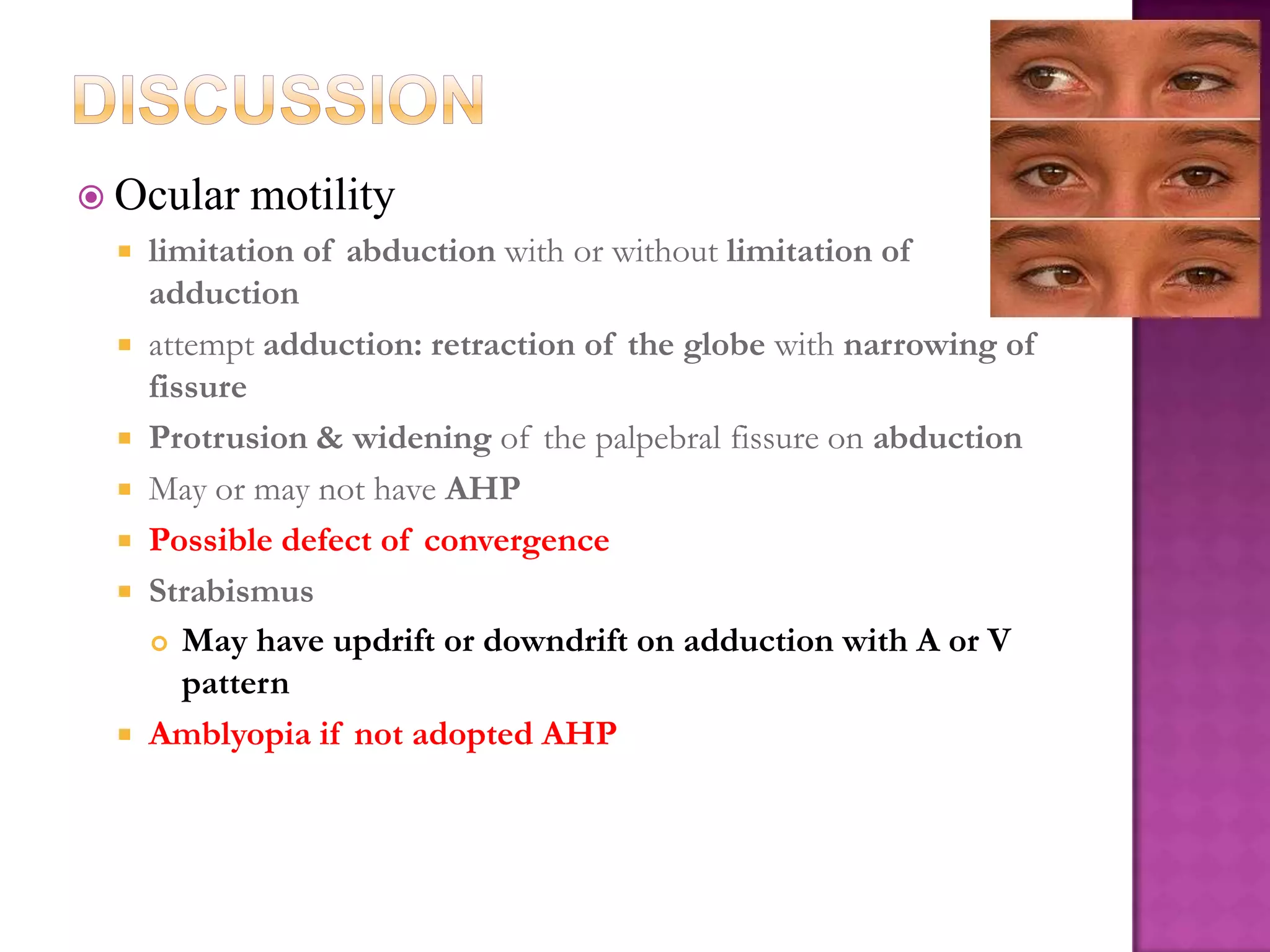
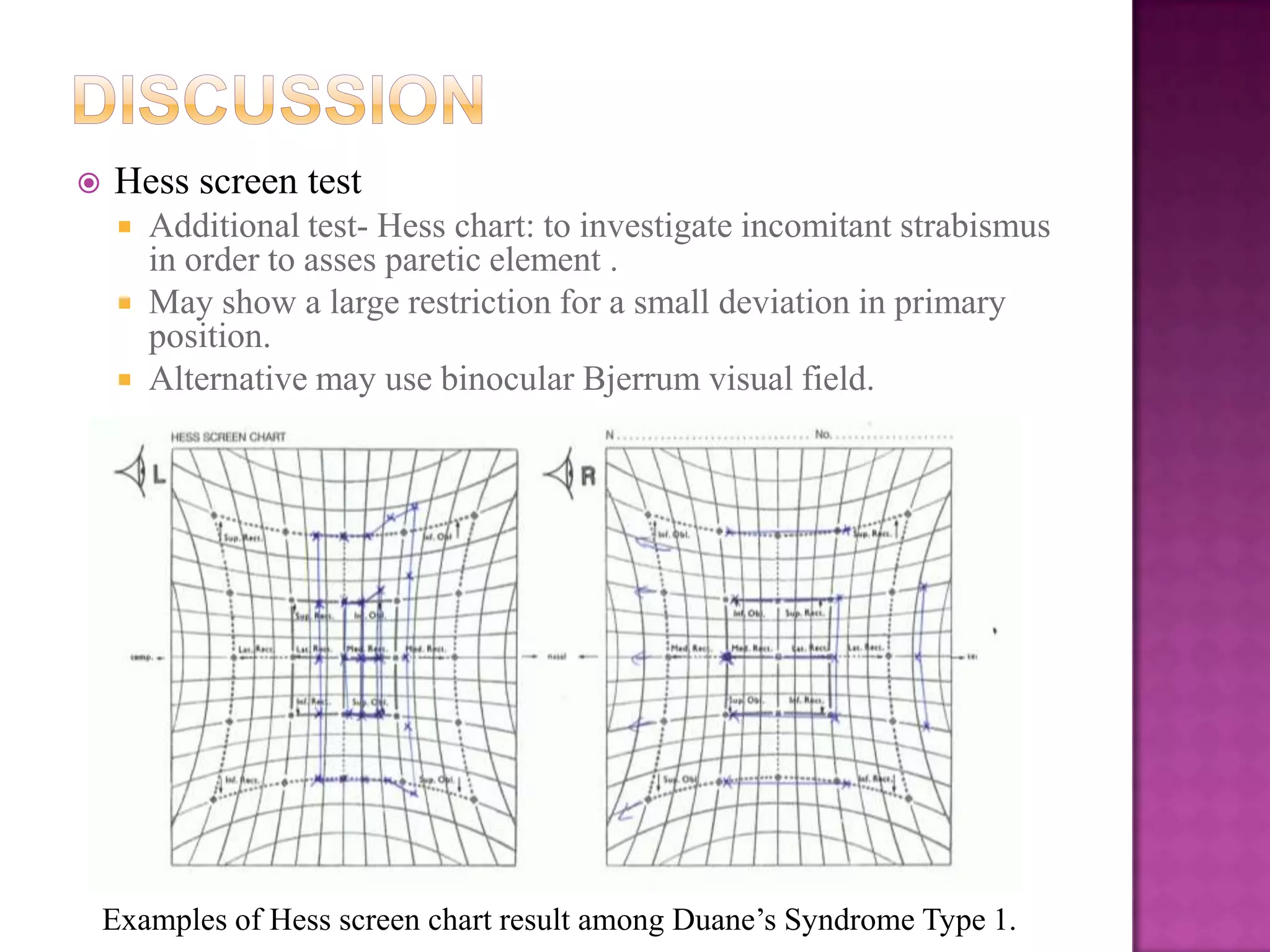
1) It is a congenital eye movement disorder caused by misdirection of eye muscle nerves, leading to abnormal eye muscle contraction.
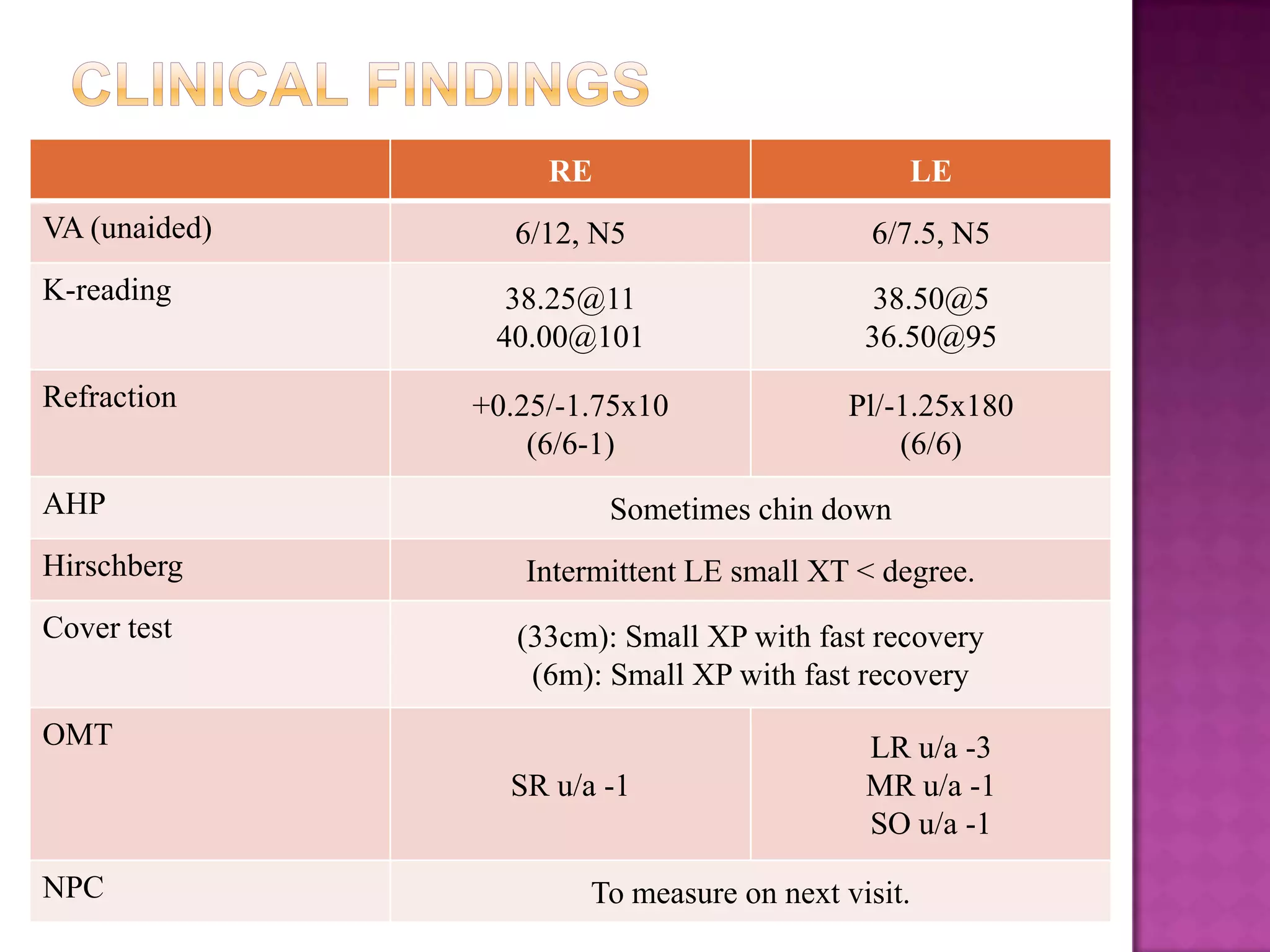
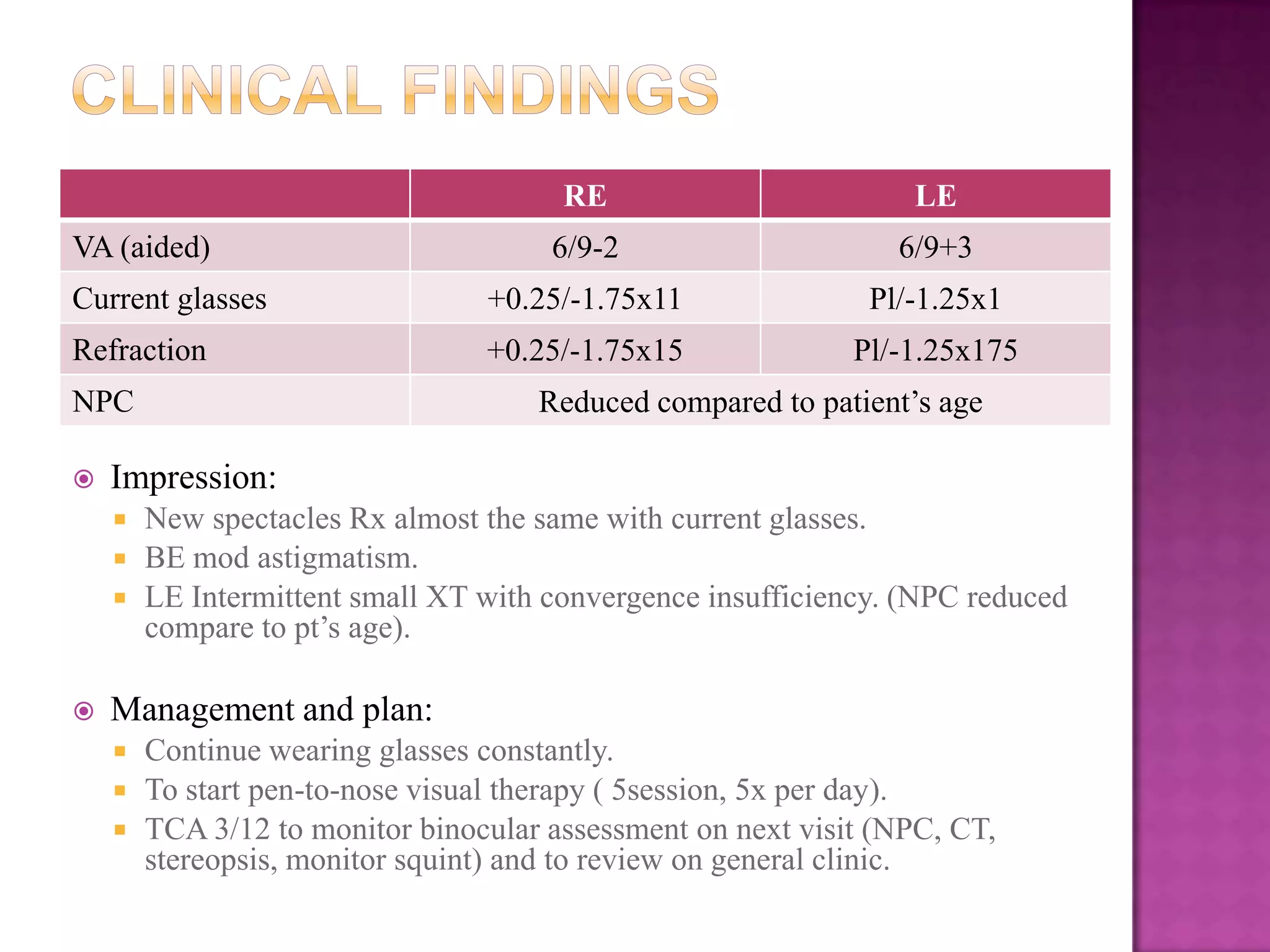
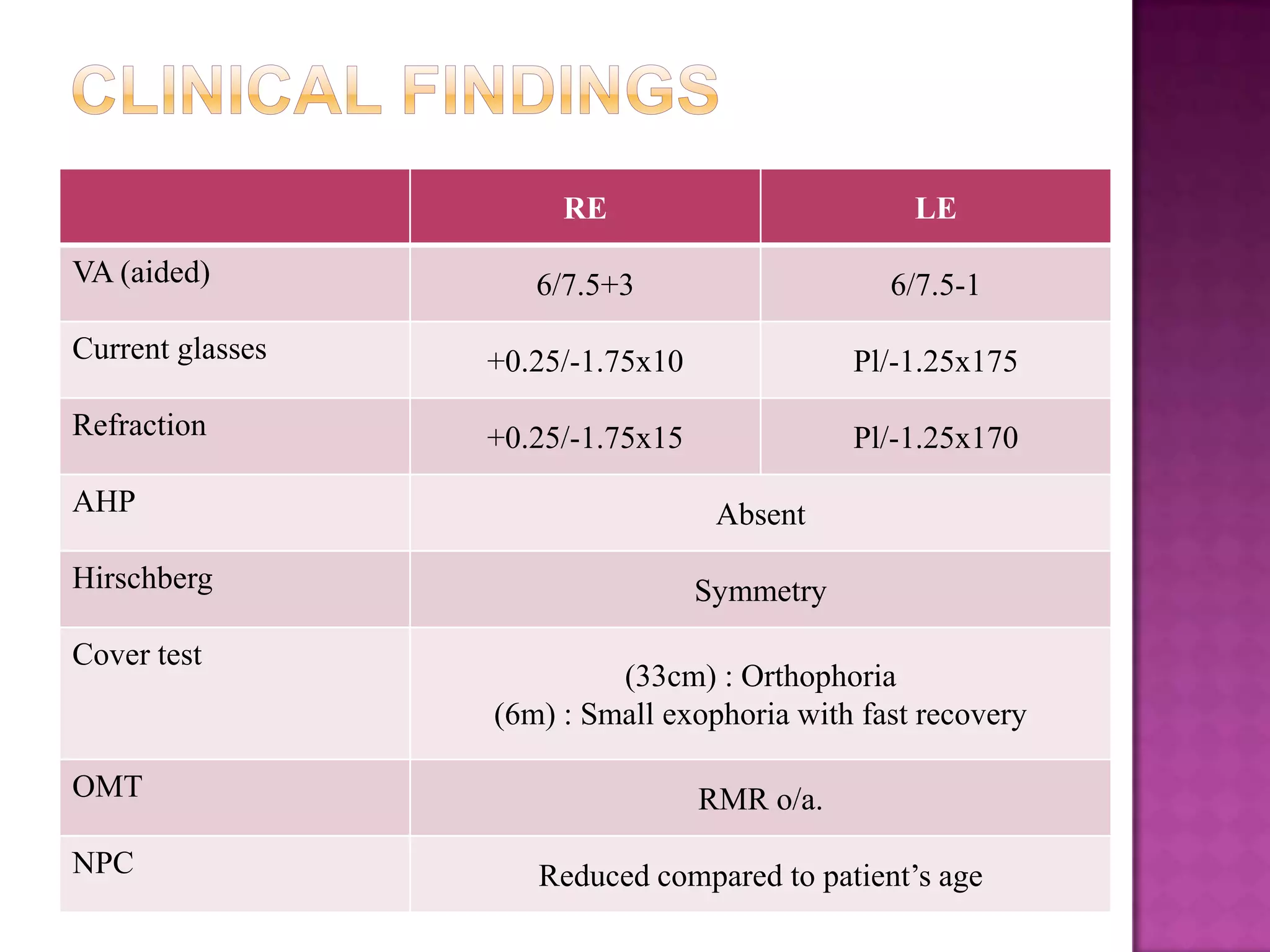
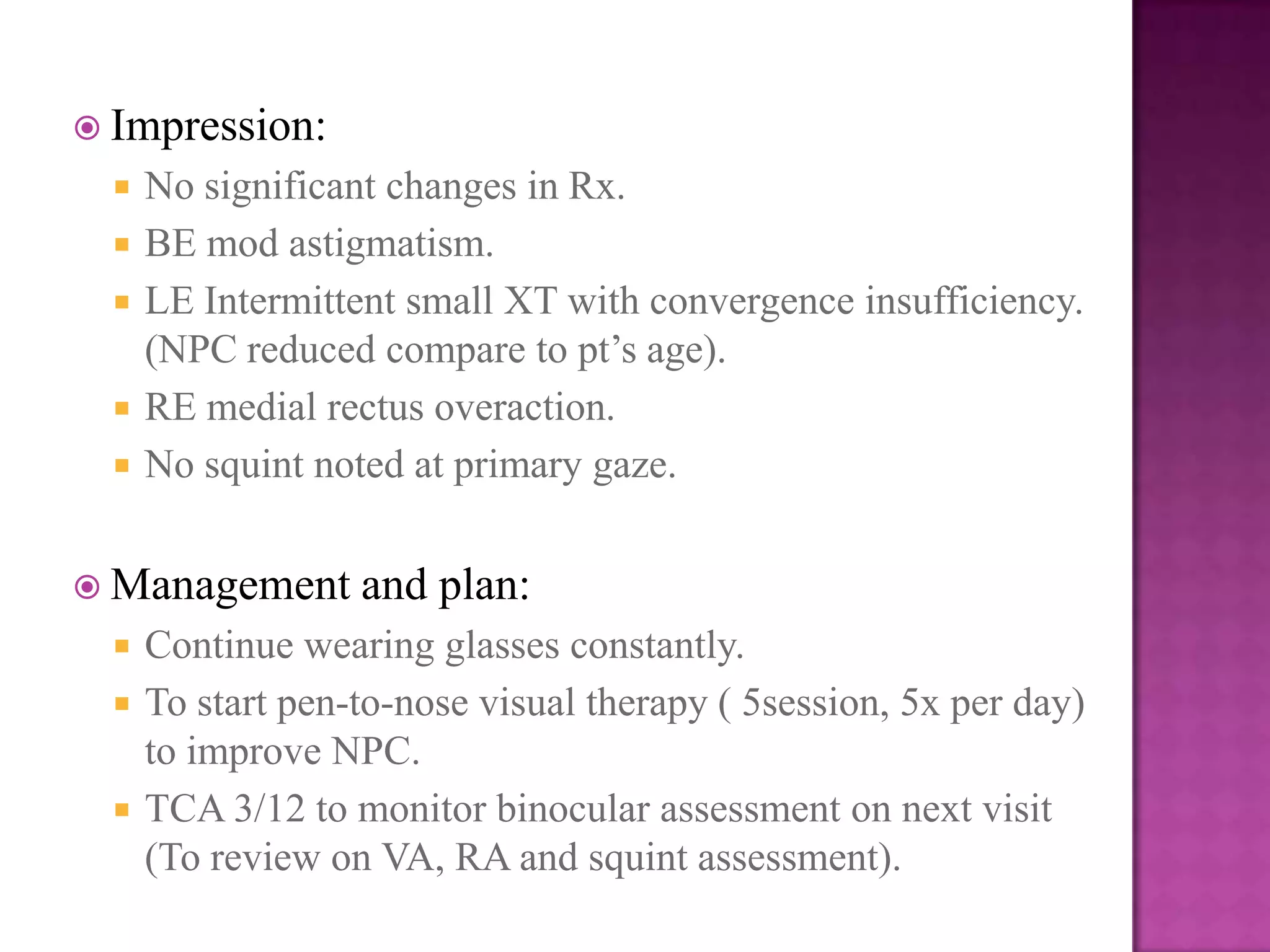
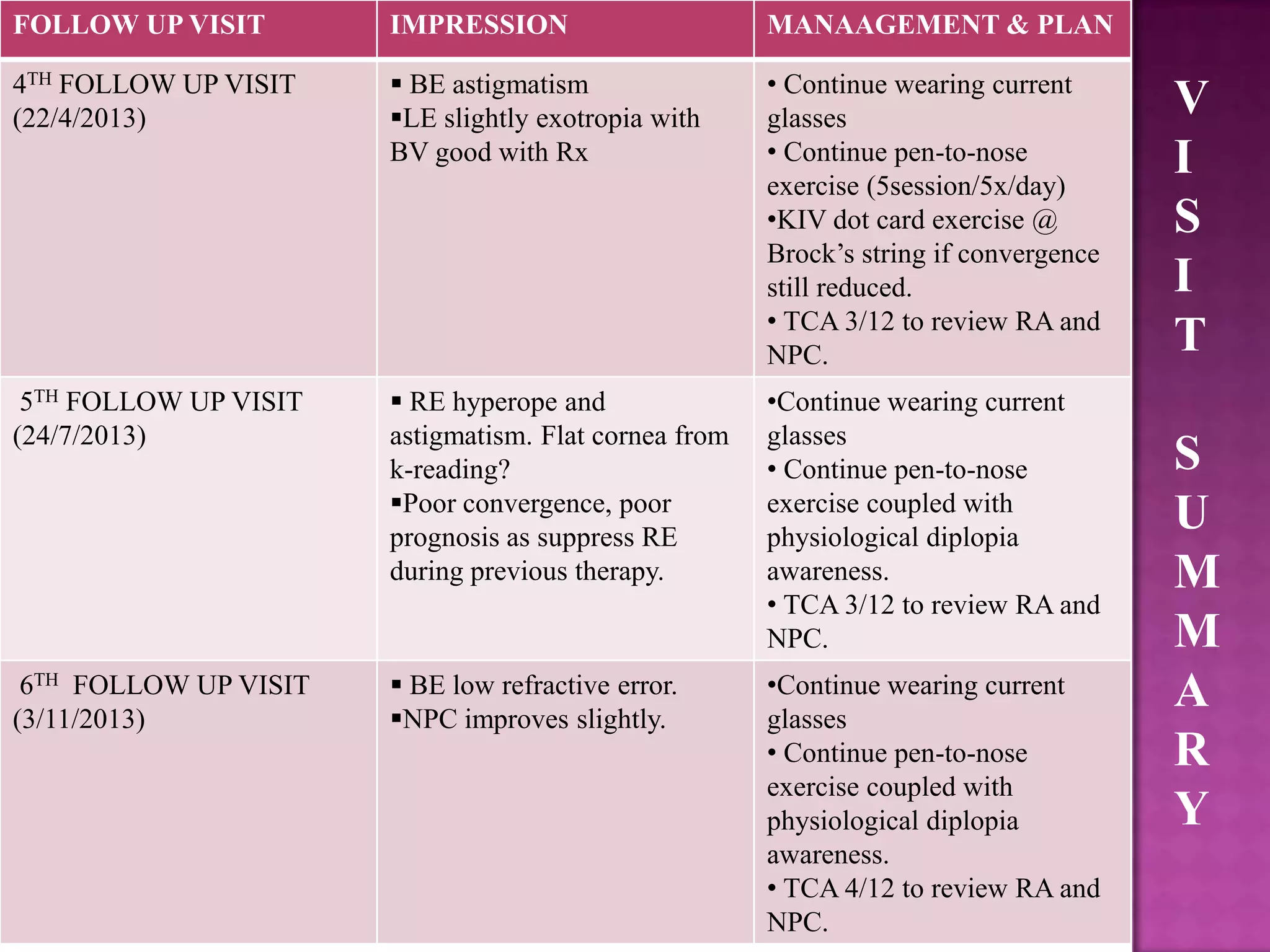
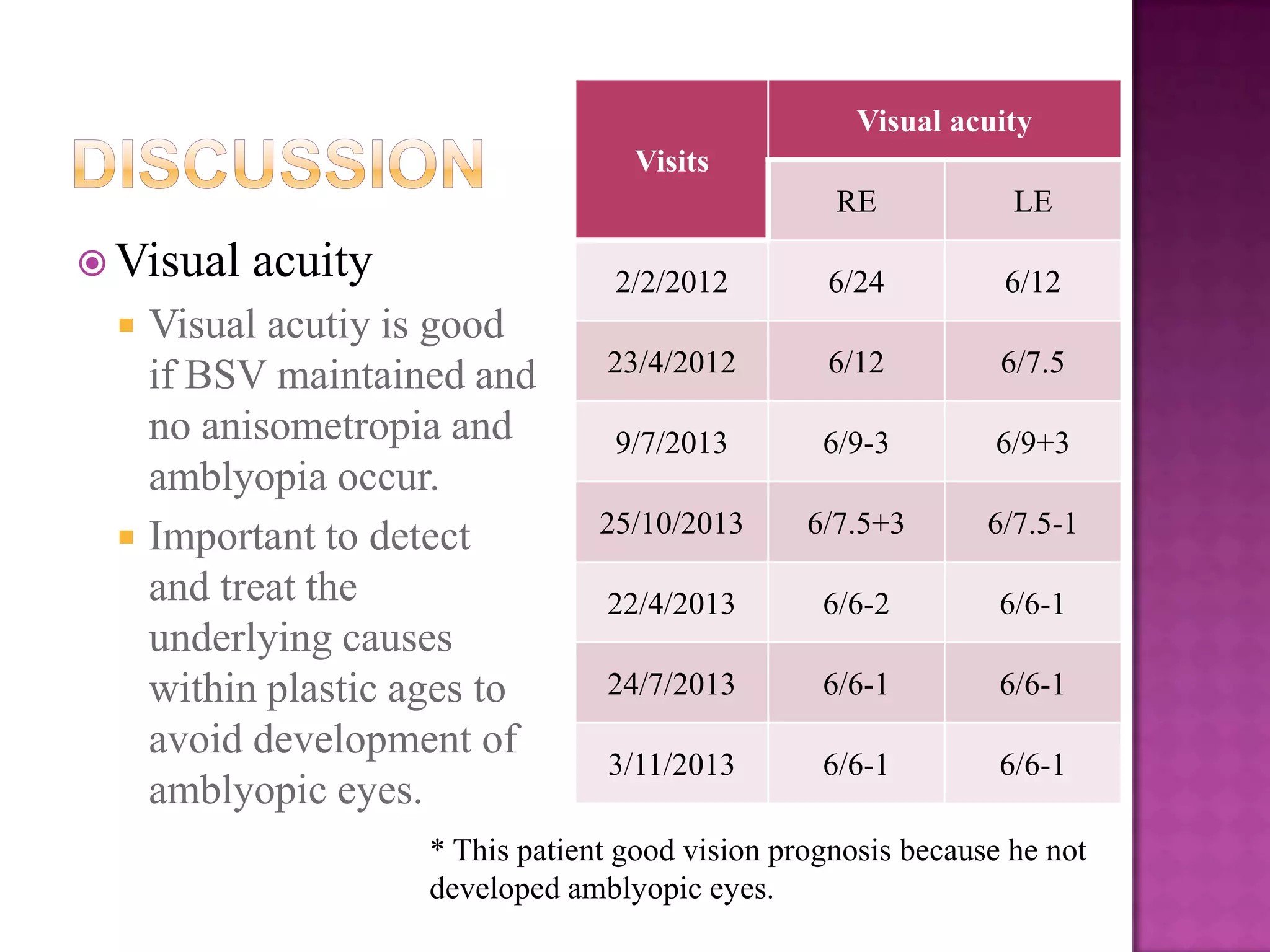
2) It affects eye abduction and retraction and can cause strabismus. Proper diagnosis and treatment are needed to prevent amblyopia.
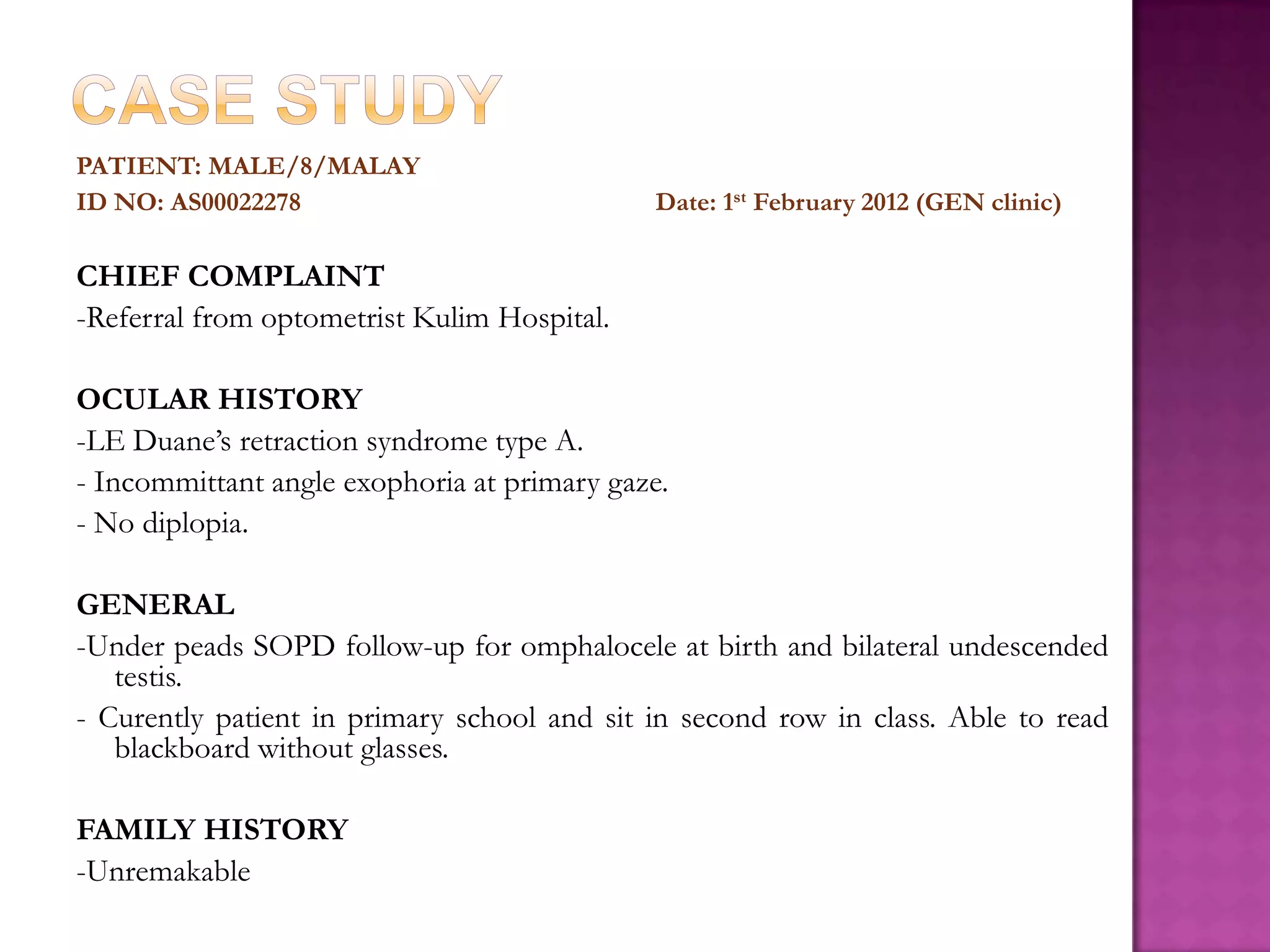
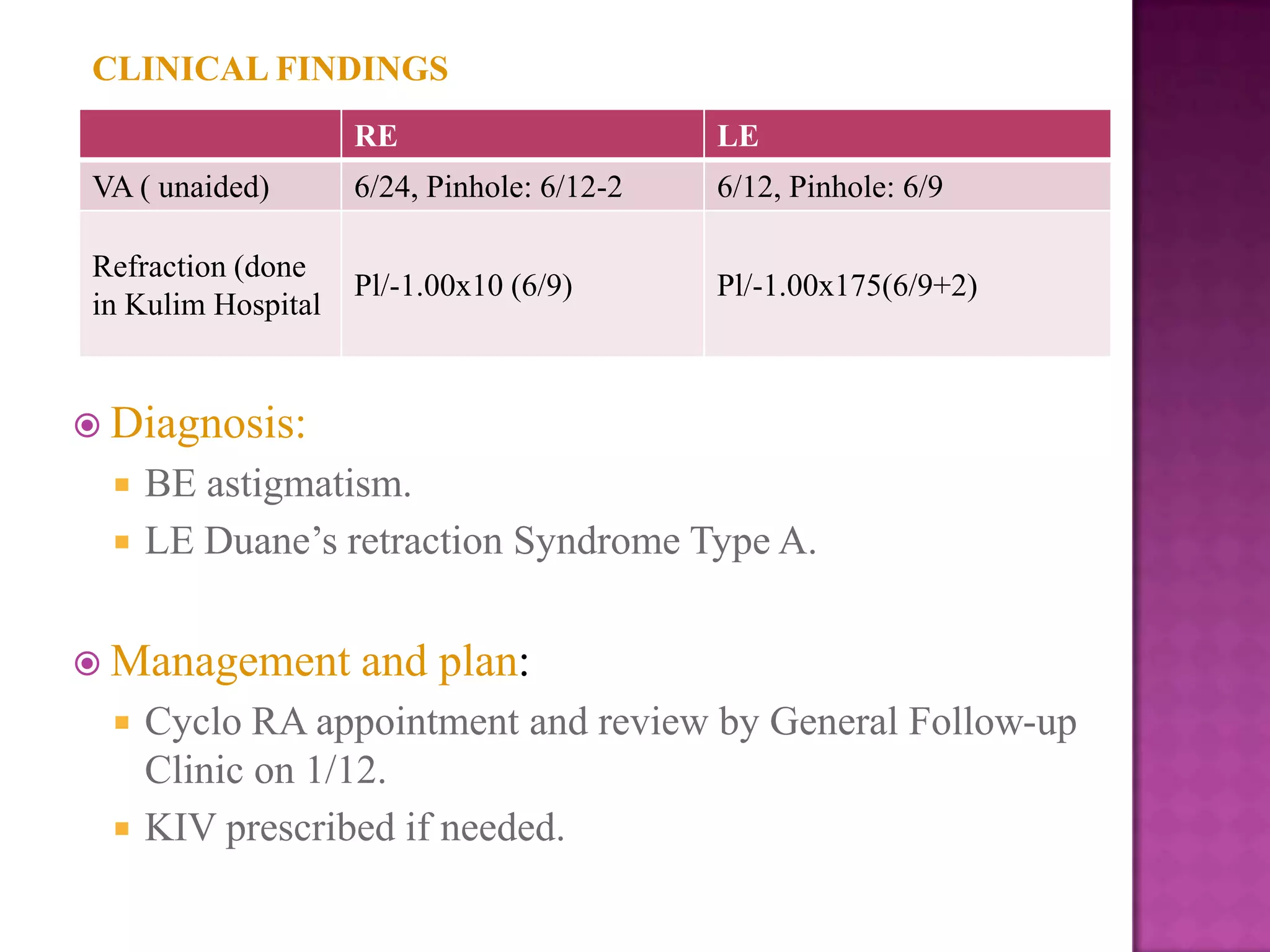
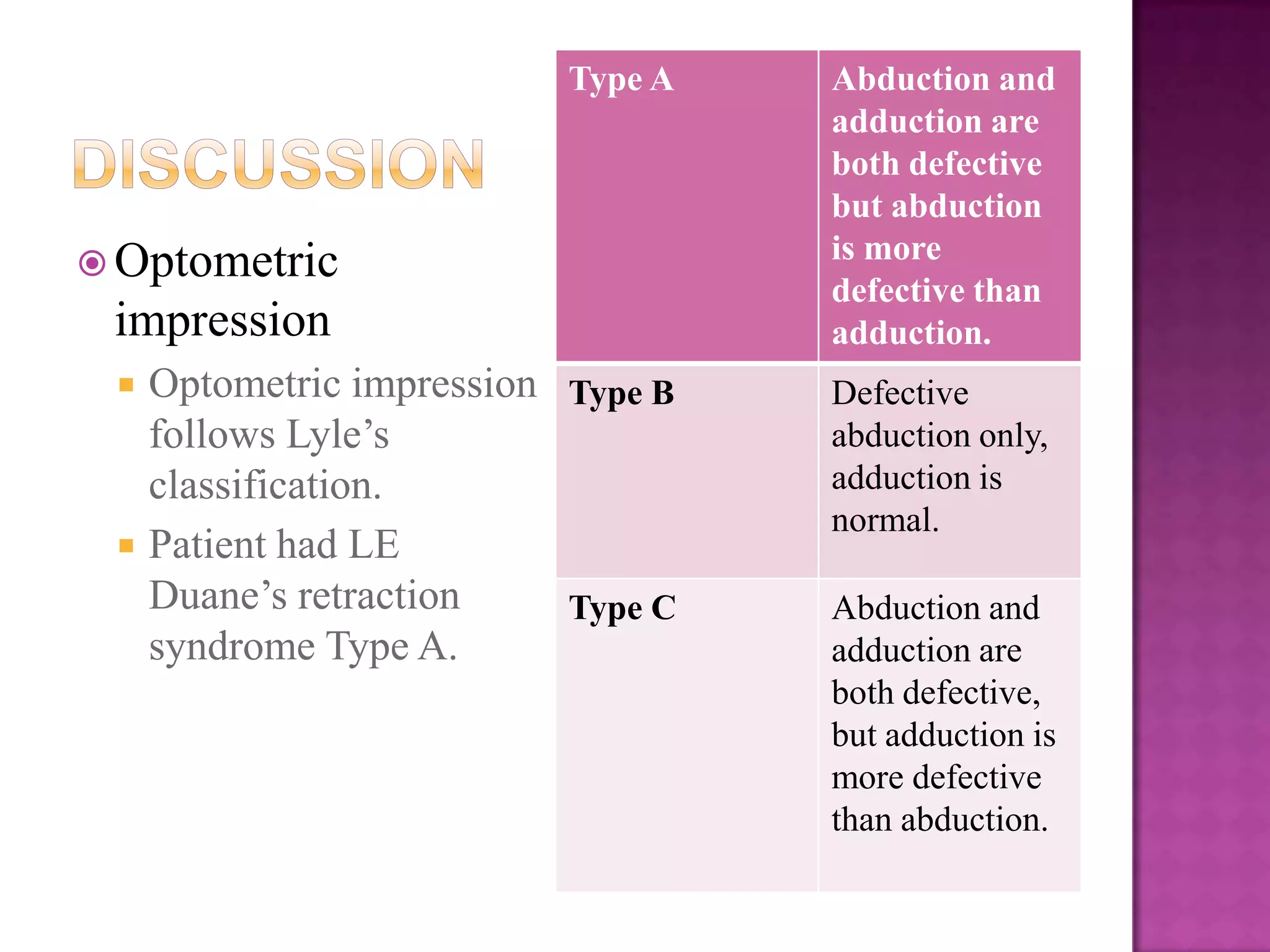
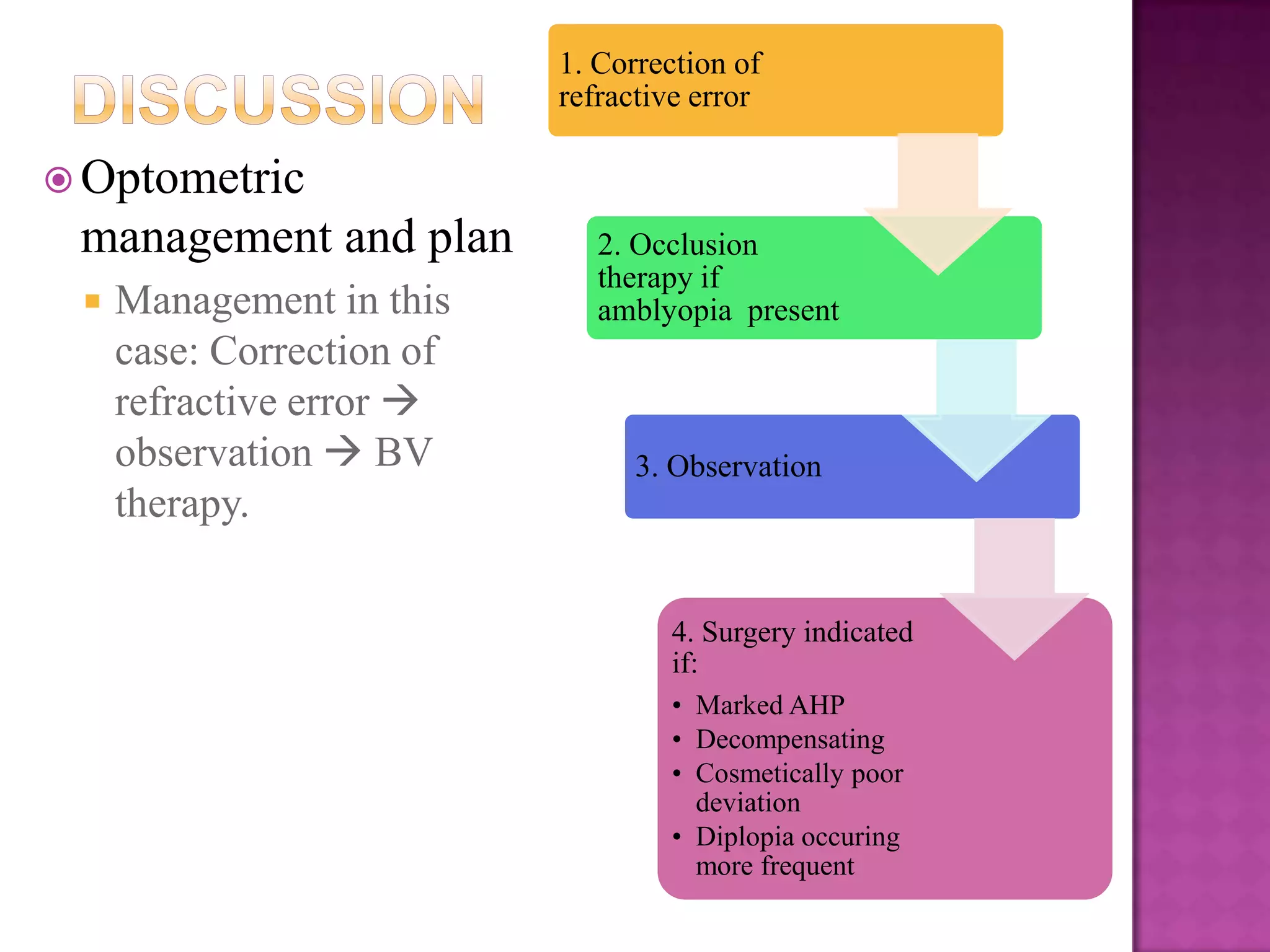
3) The case study describes a young male patient with left eye Duane's syndrome type 1 who was properly managed with glasses and vision therapy to maintain good vision outcomes.