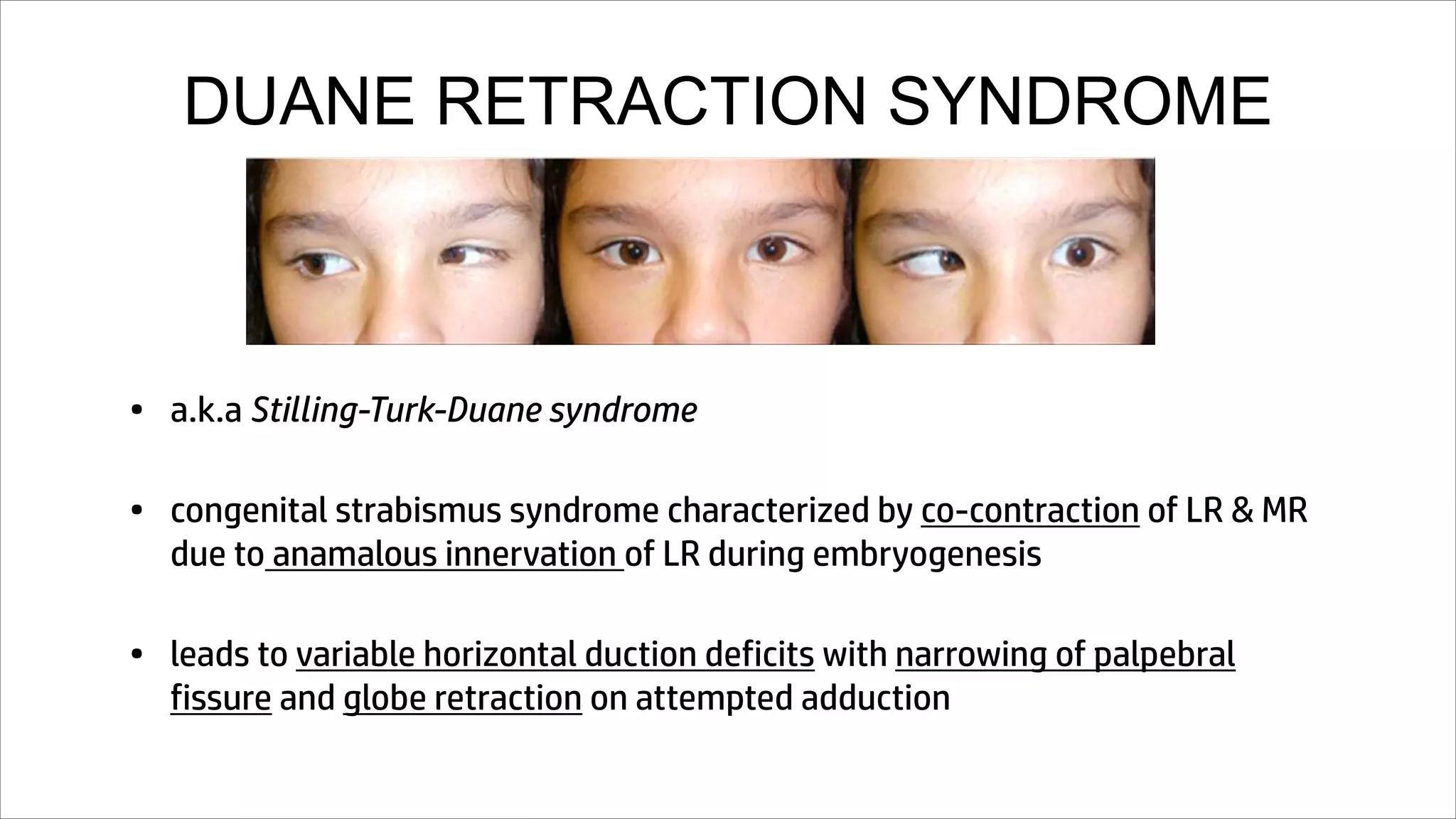
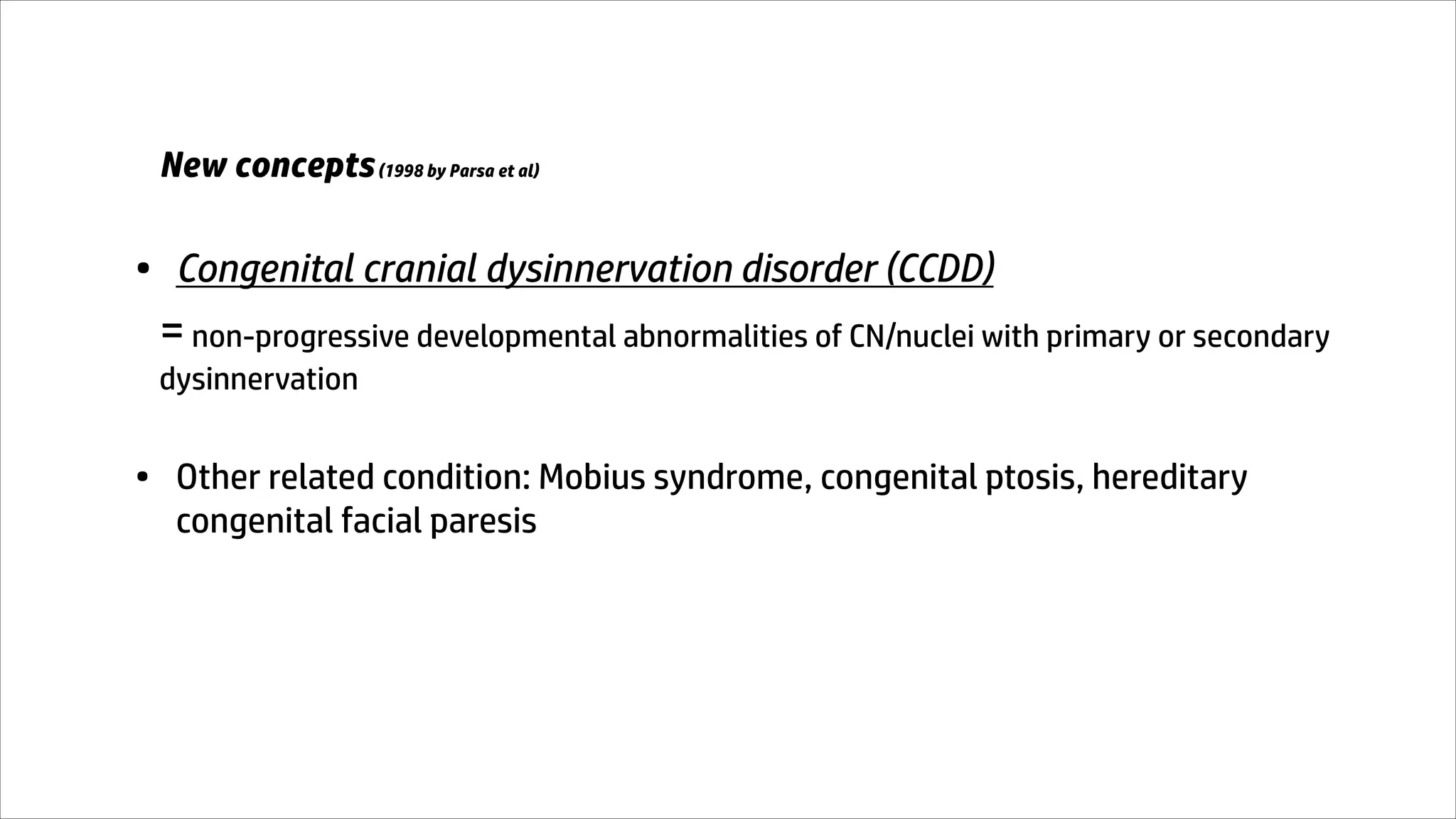
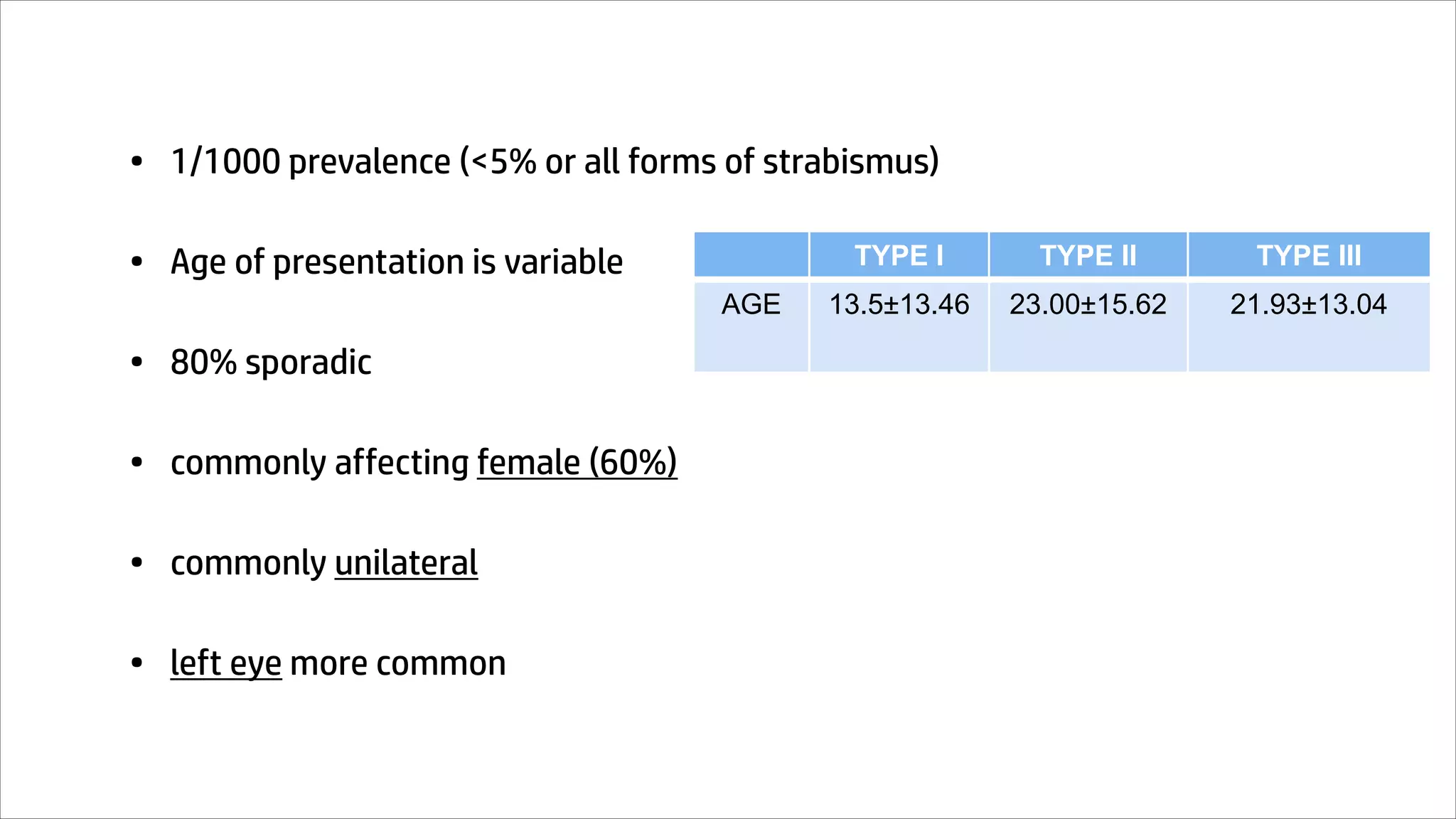
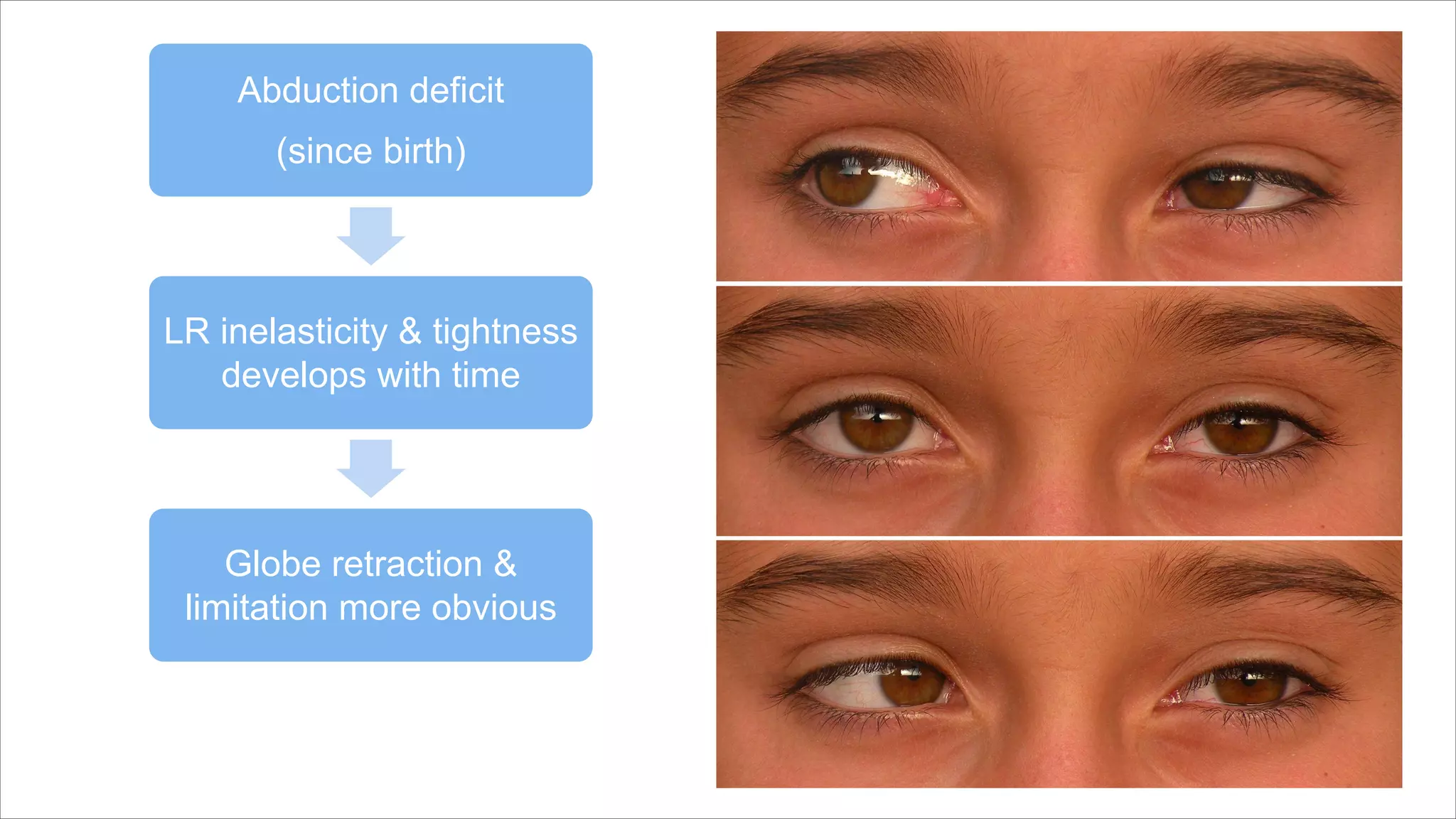
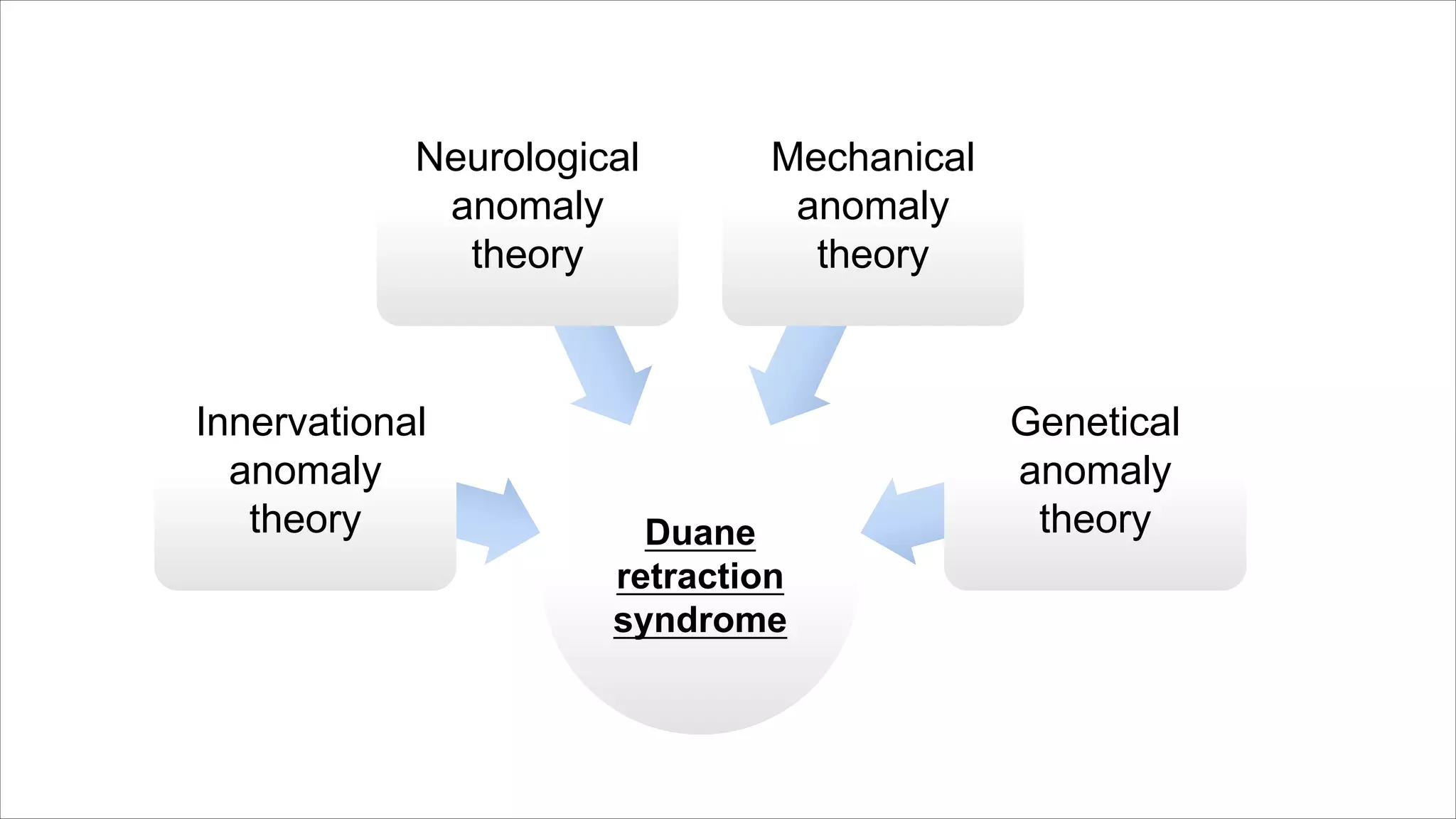
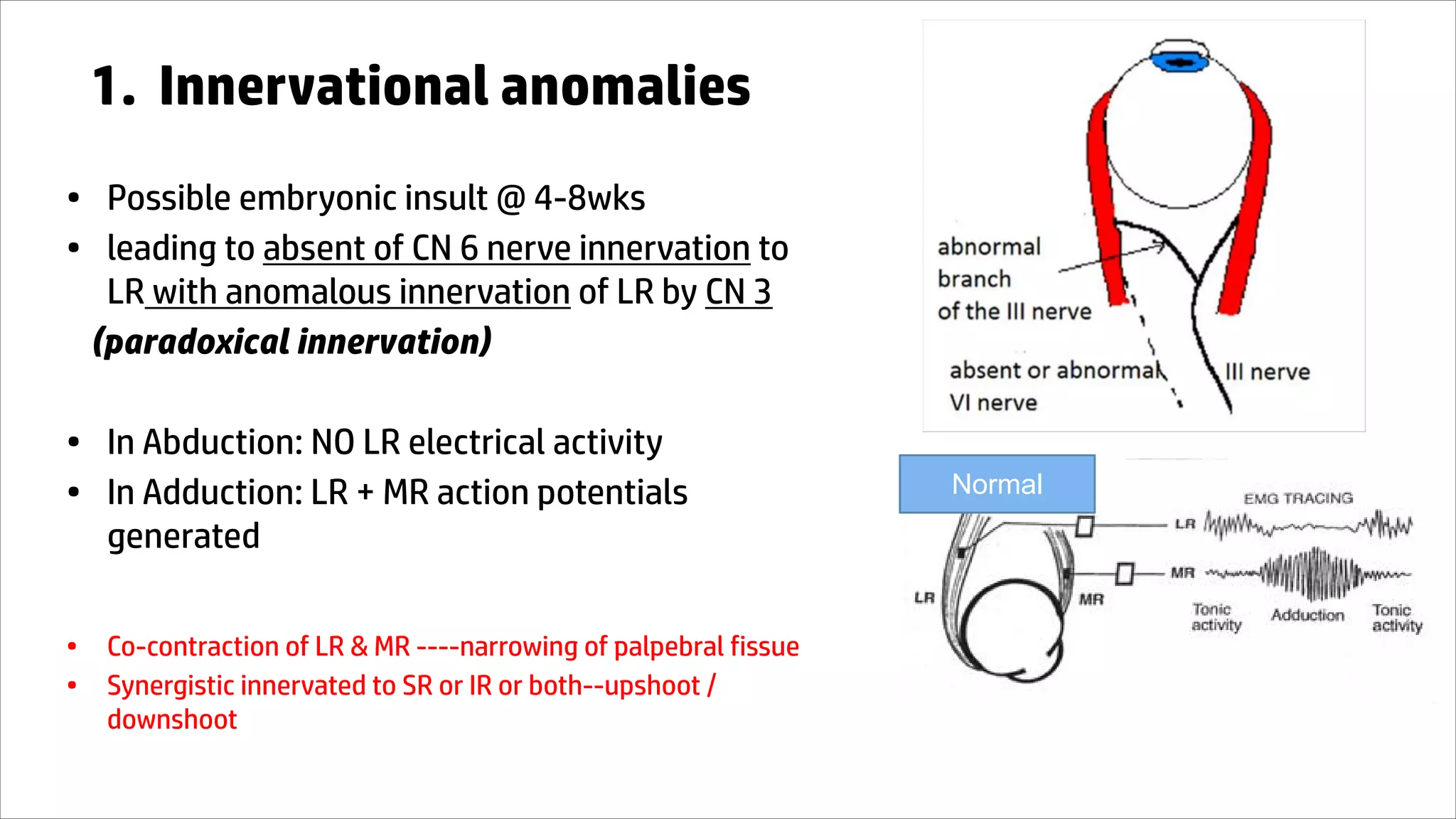
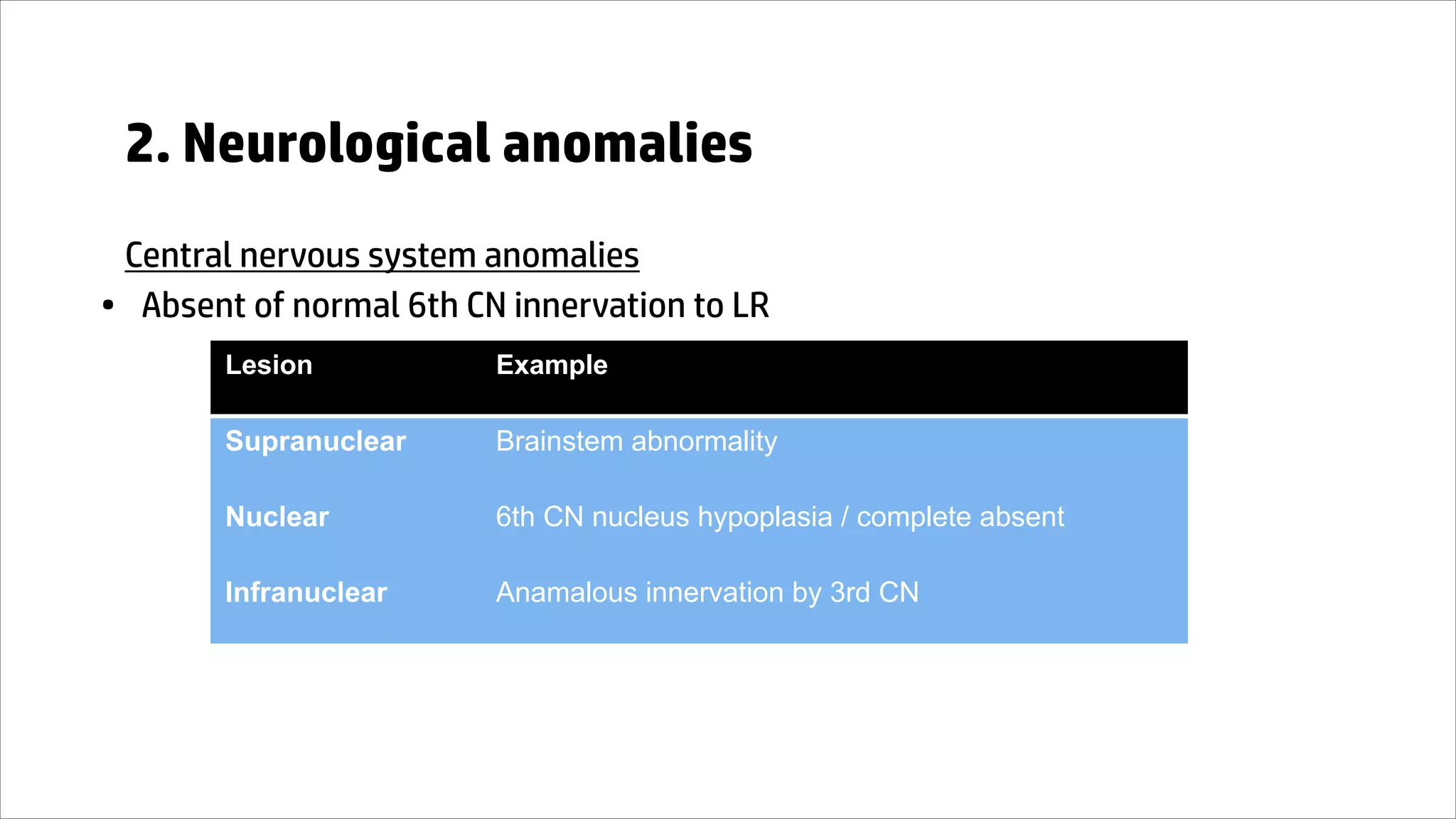
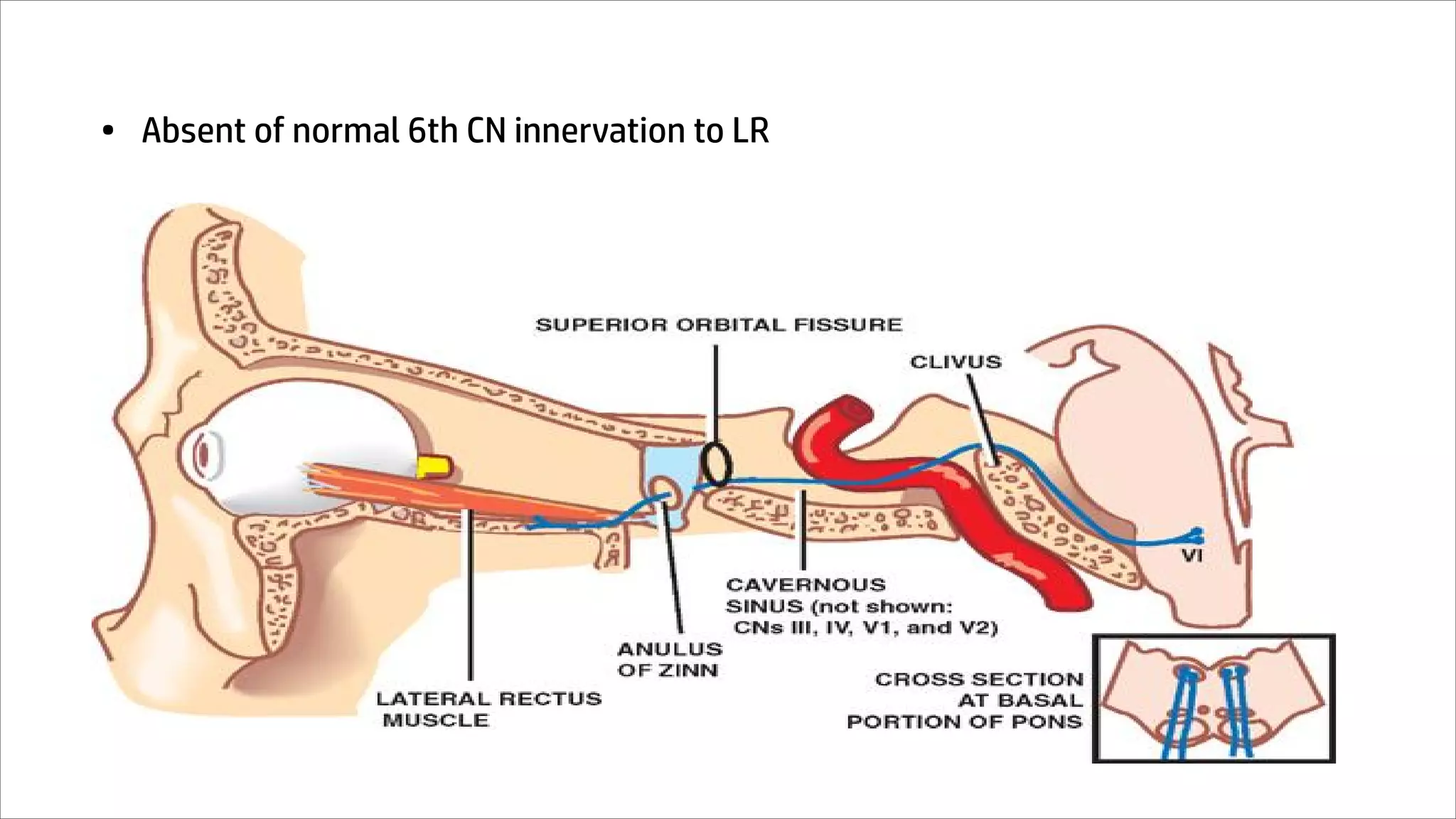
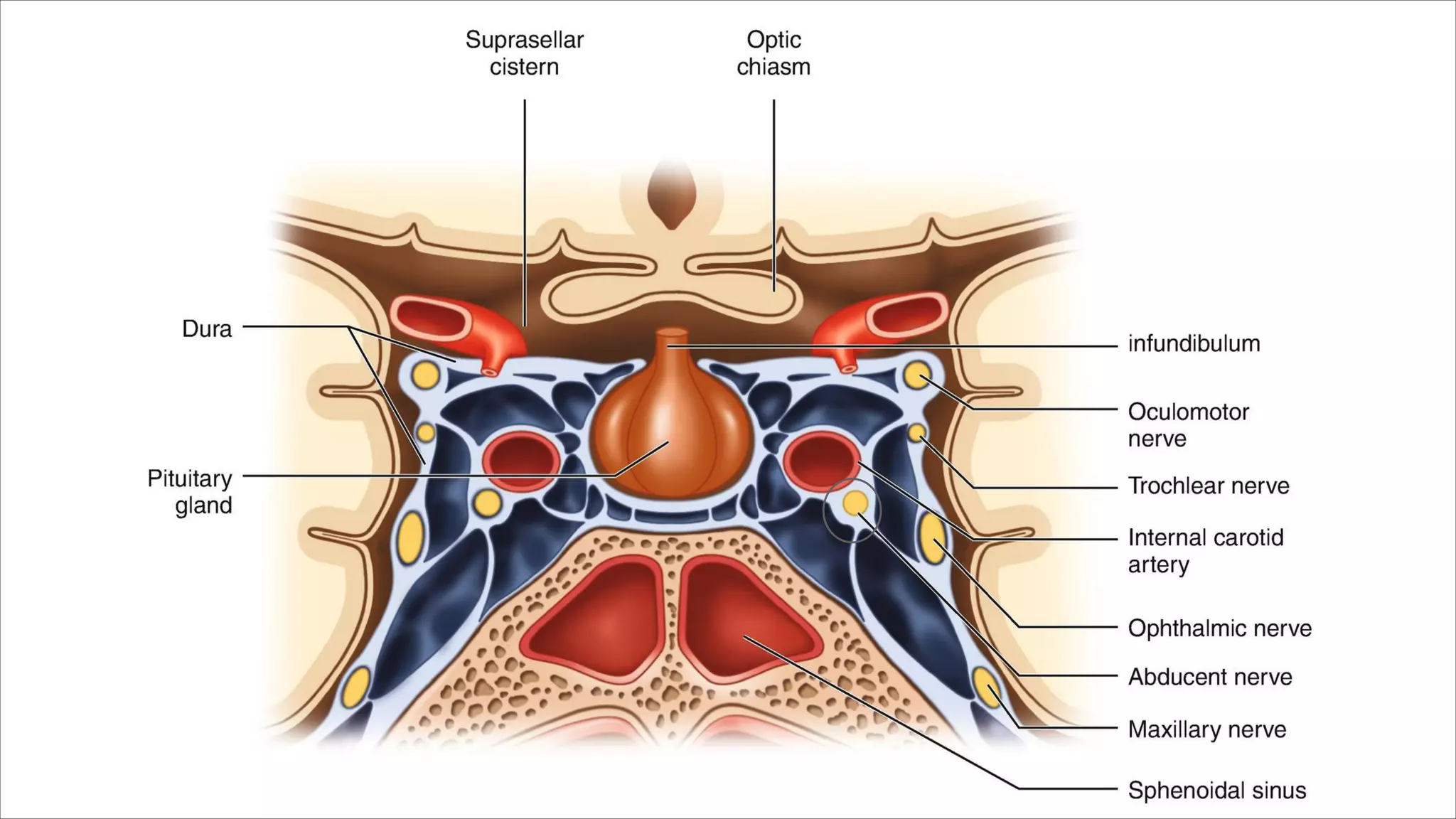
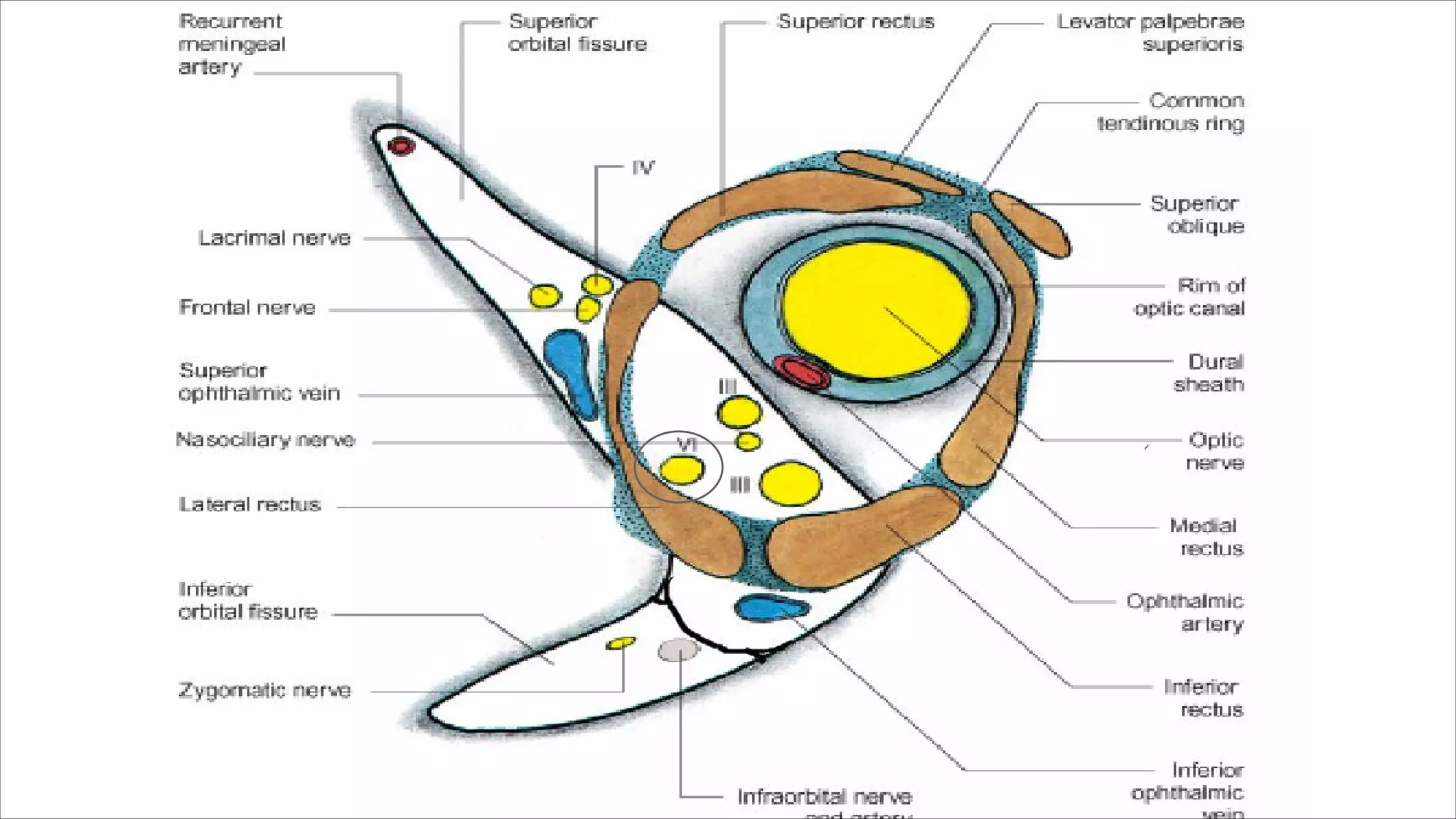
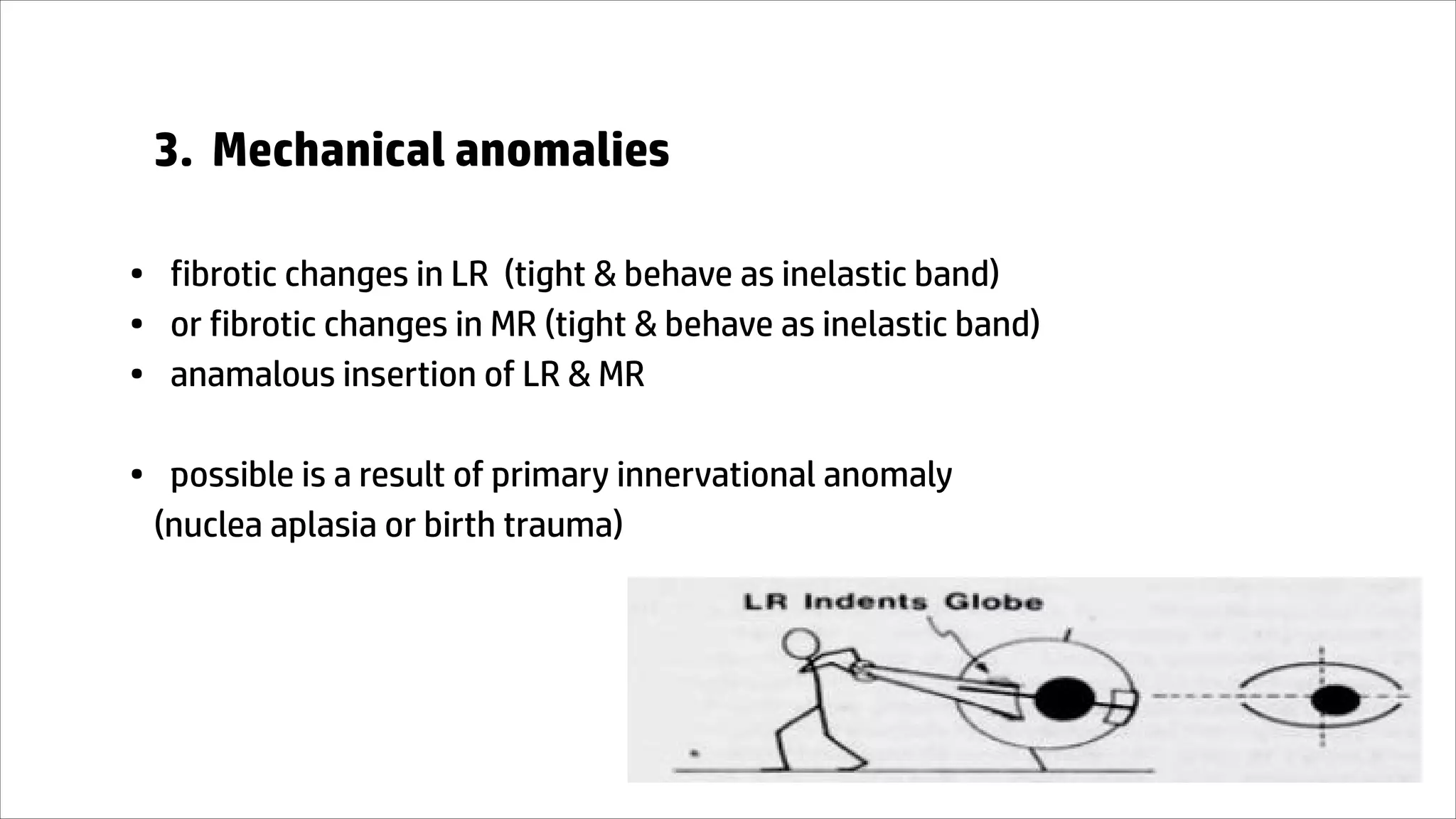
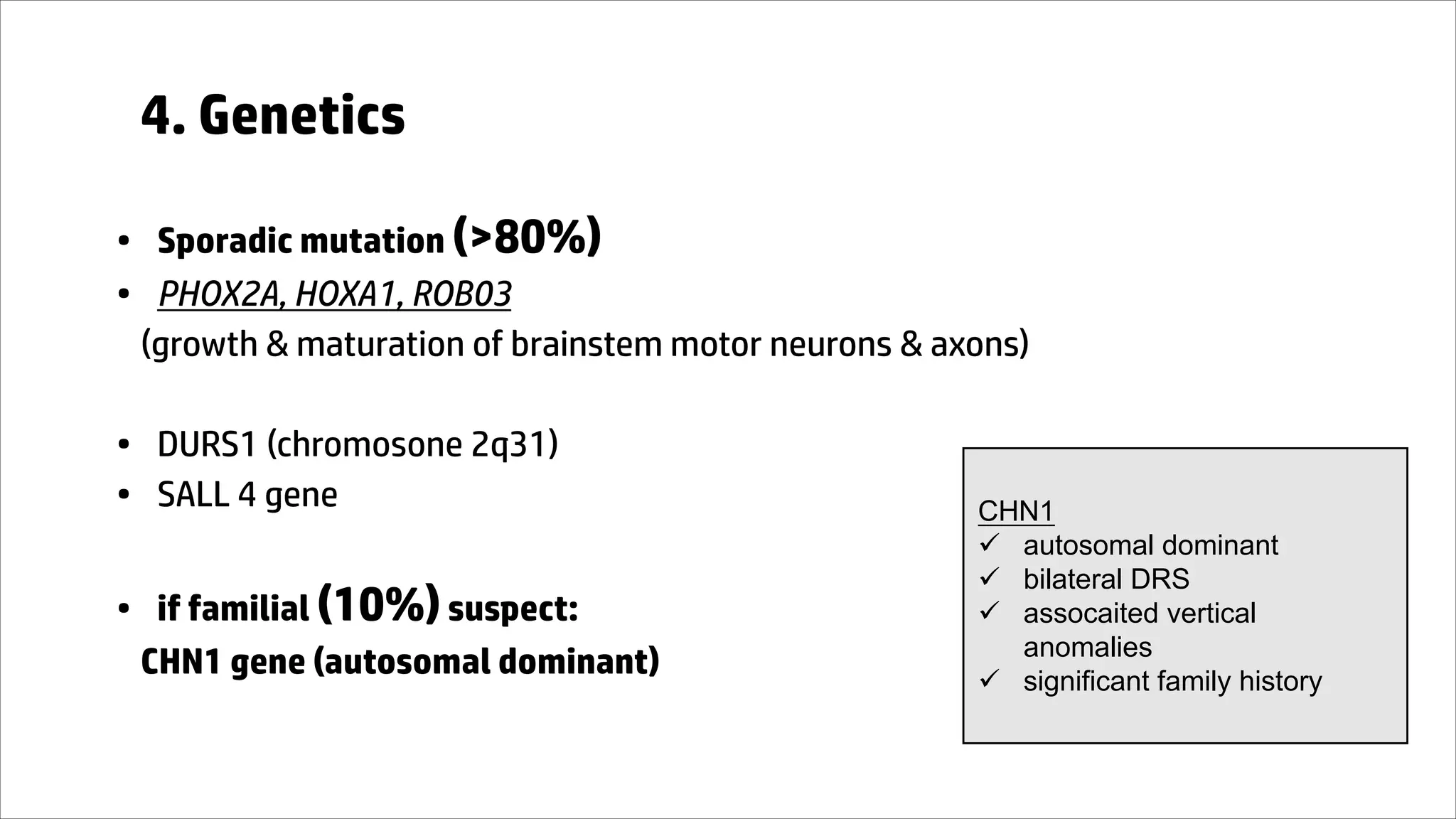
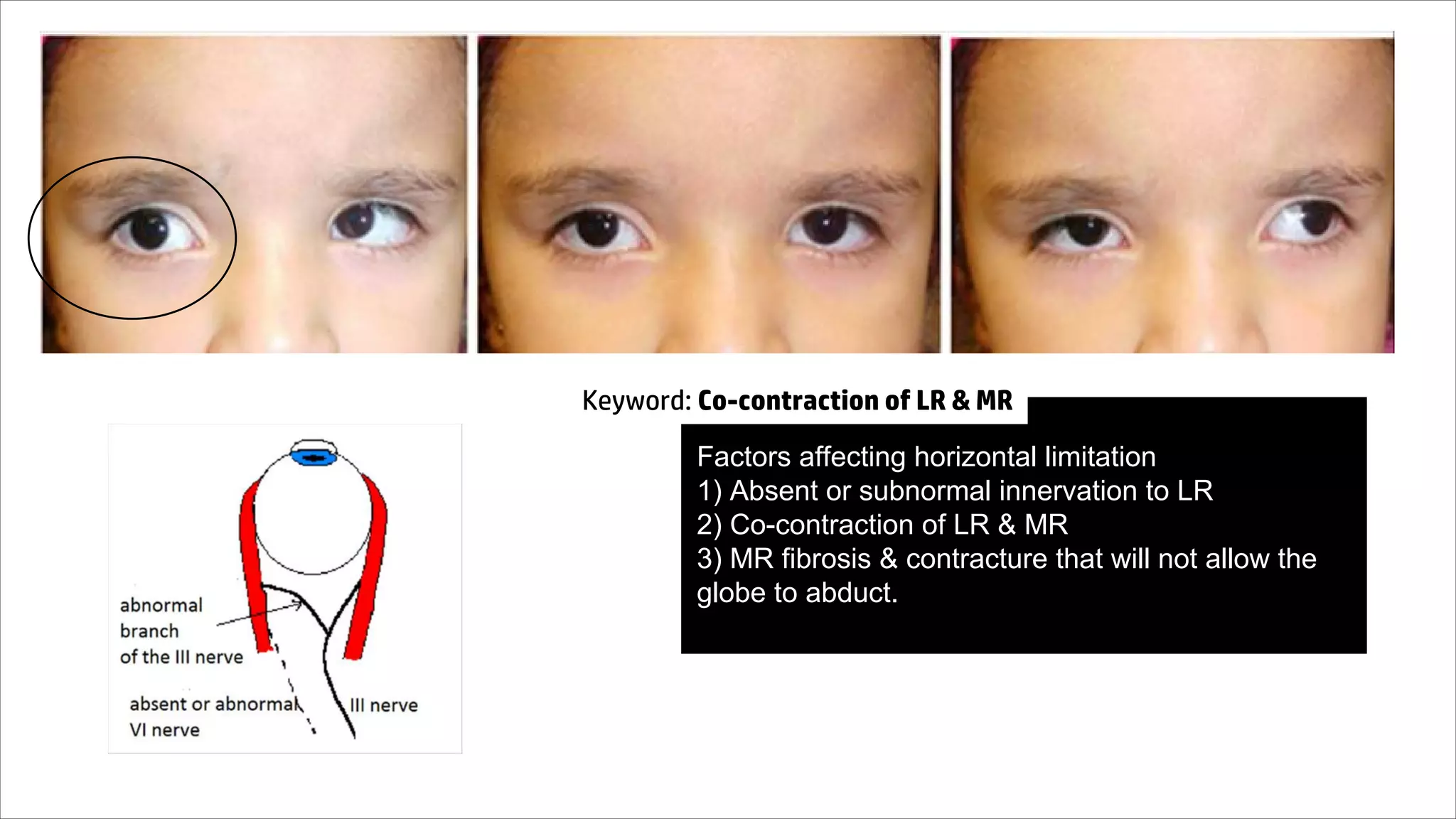
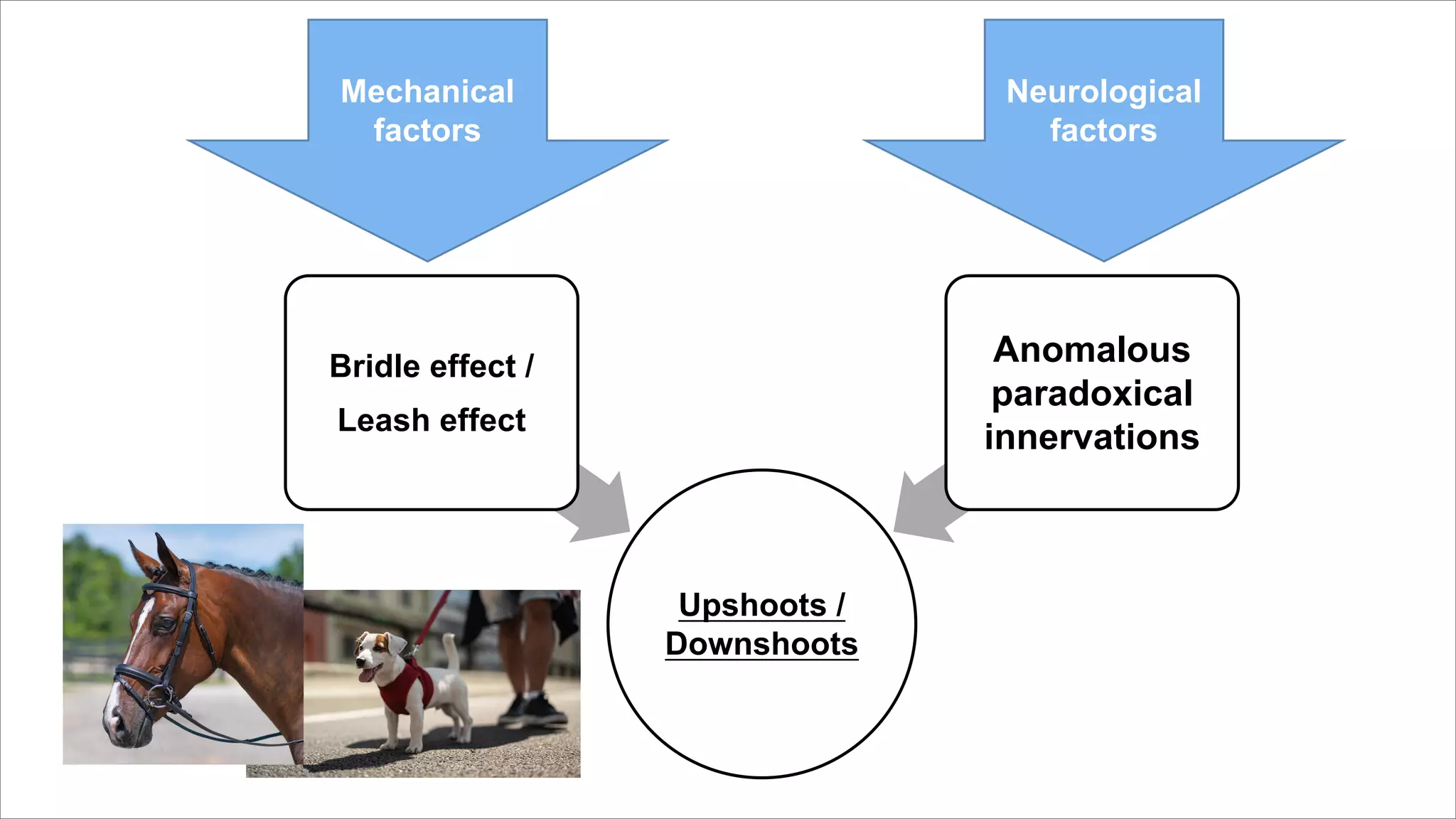
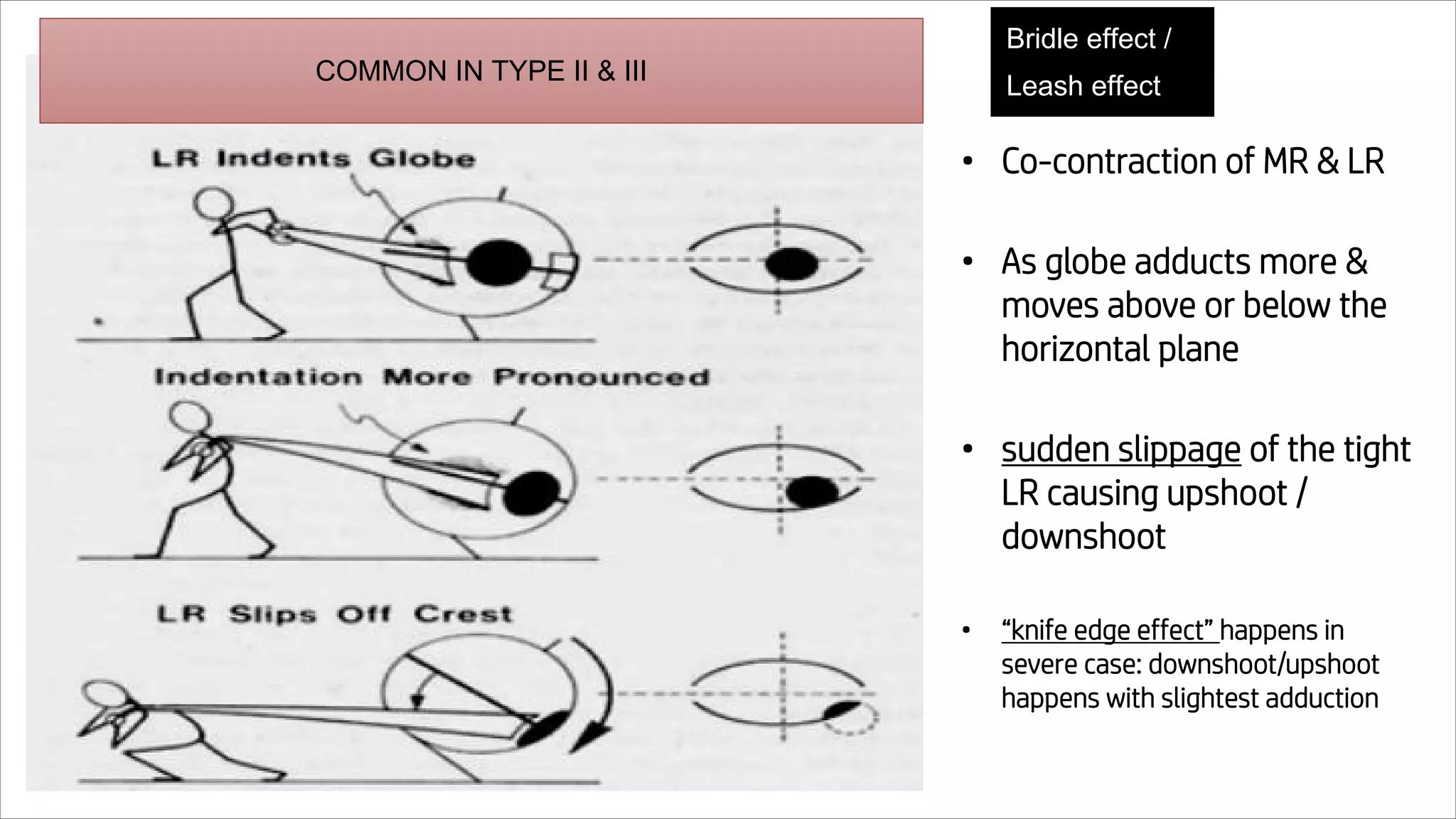
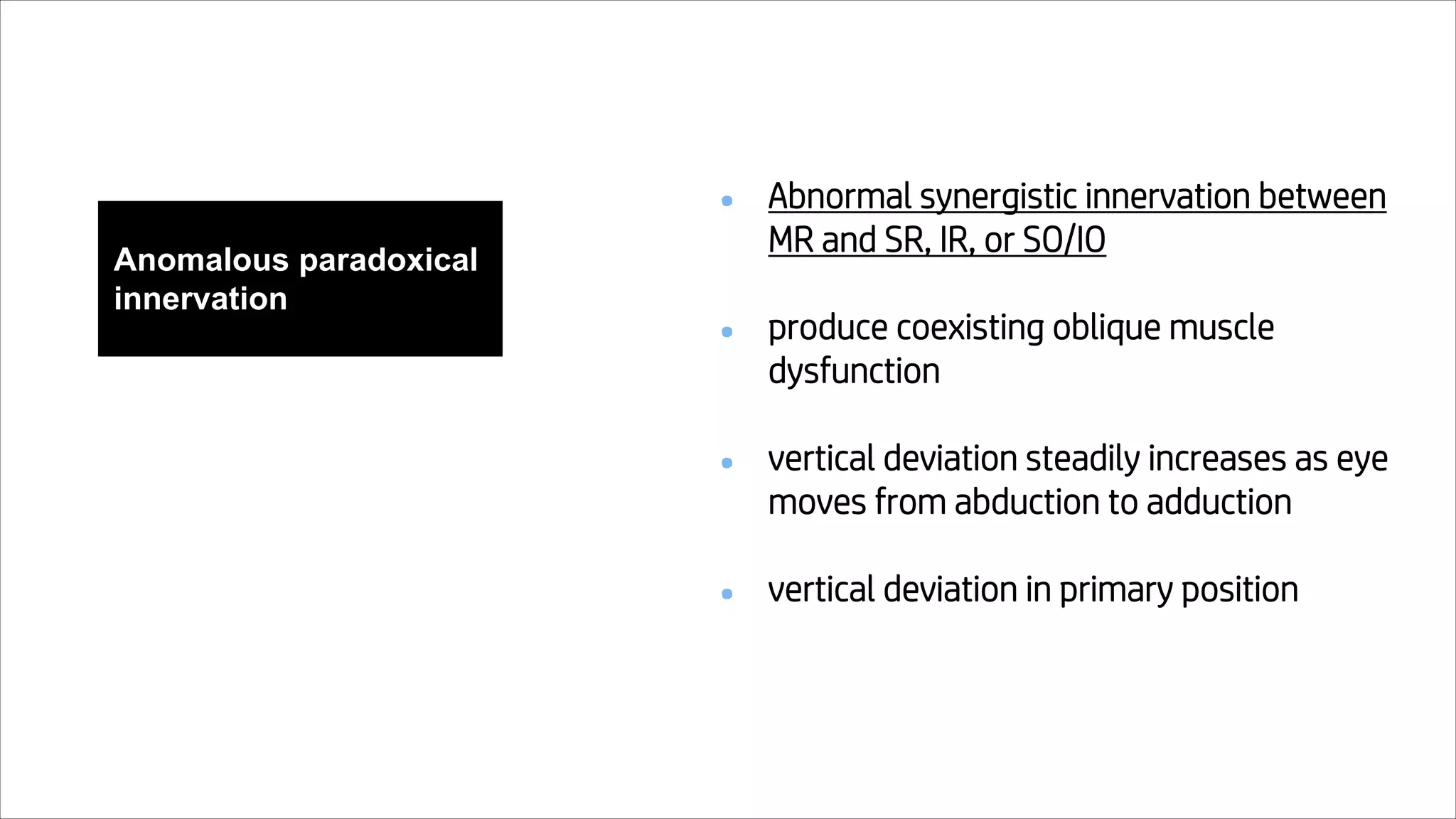
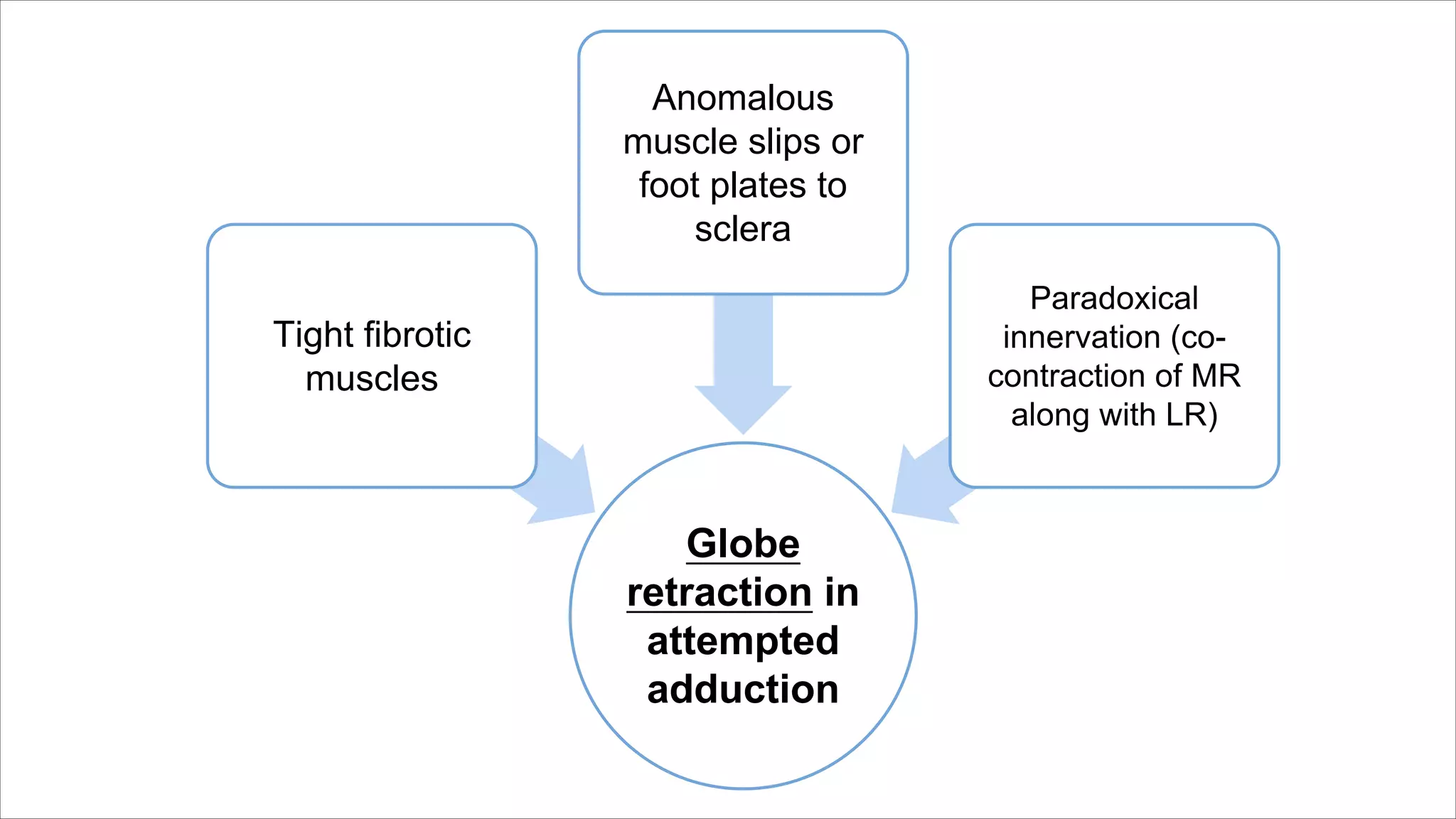
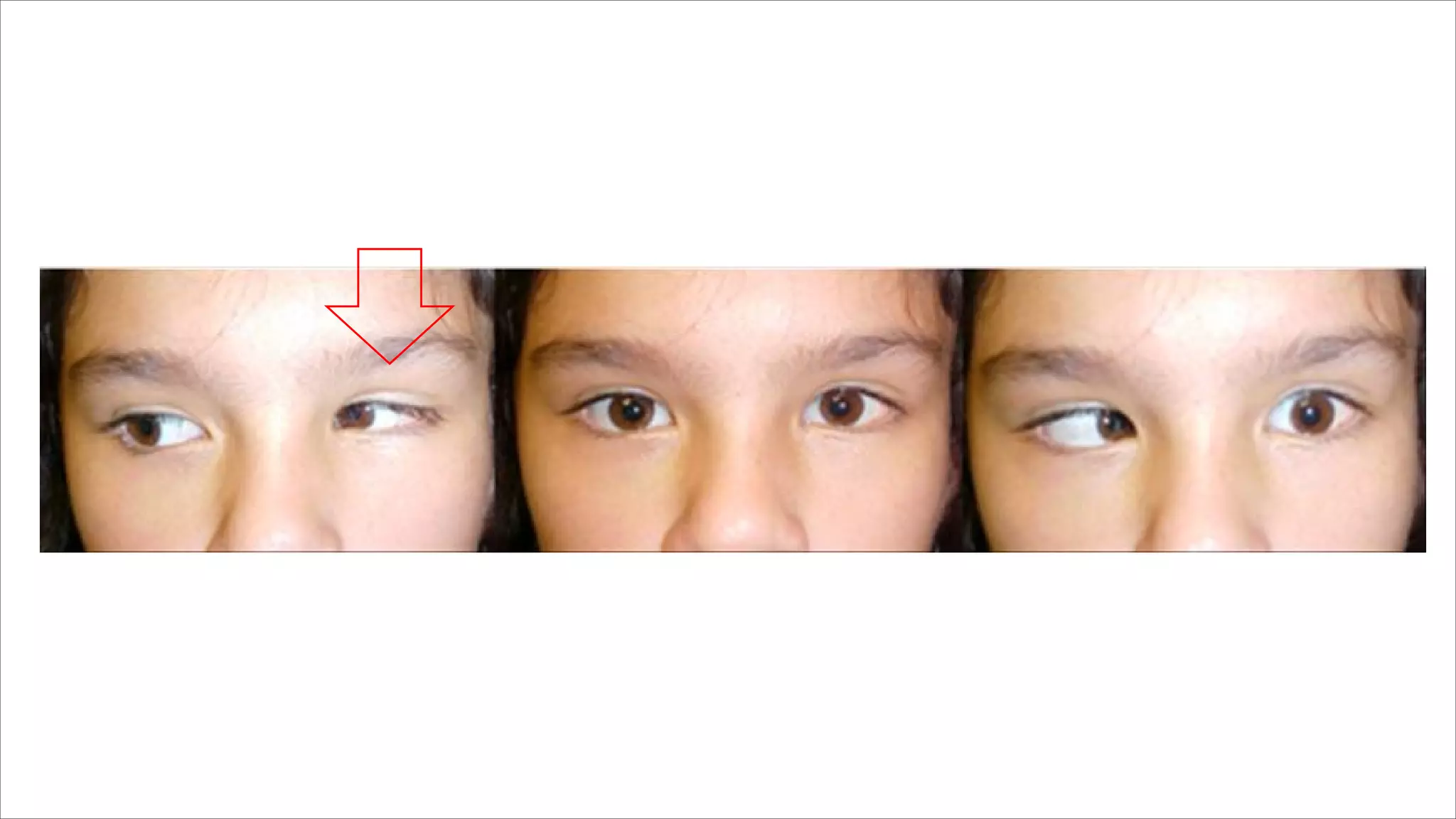
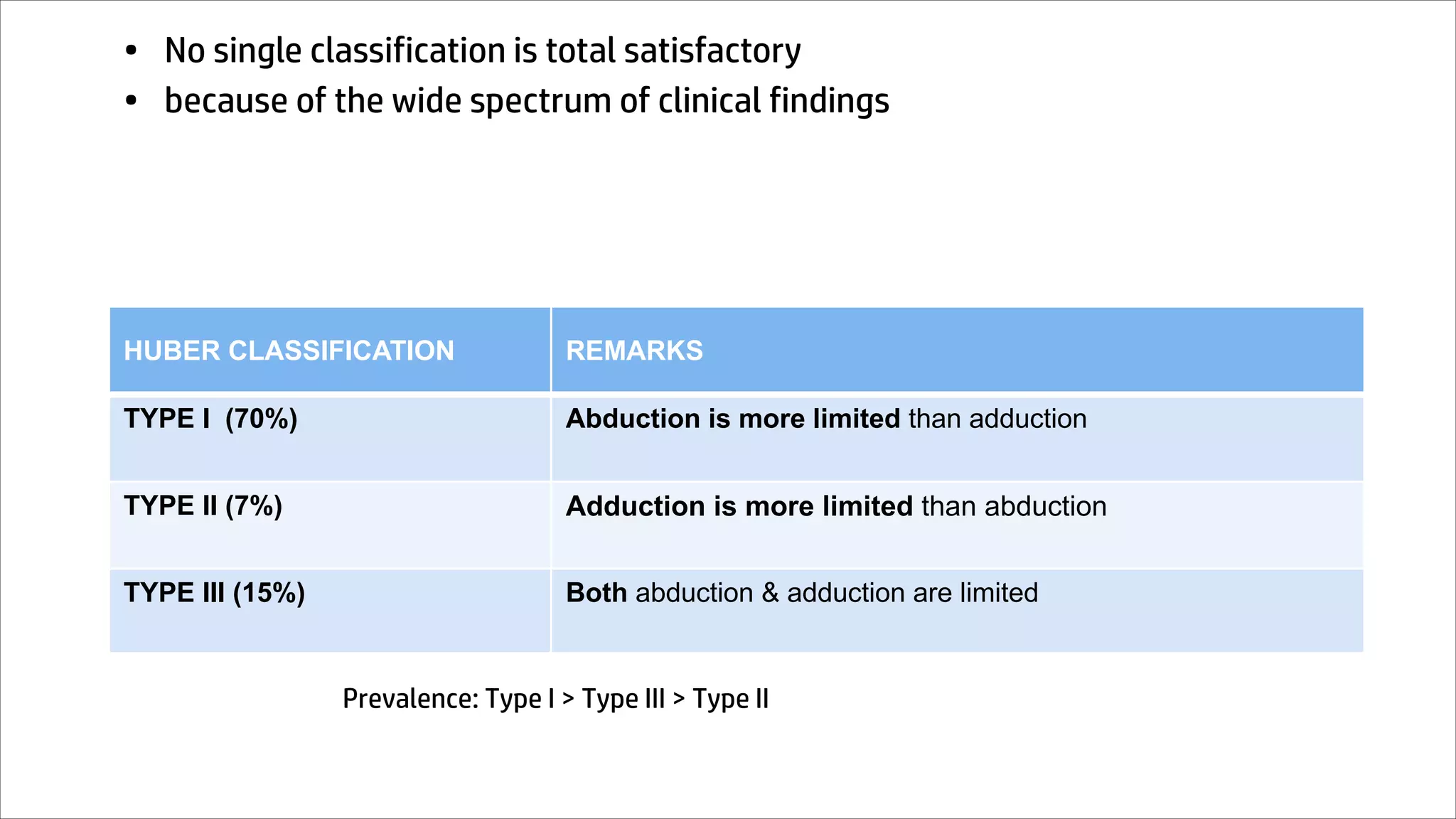
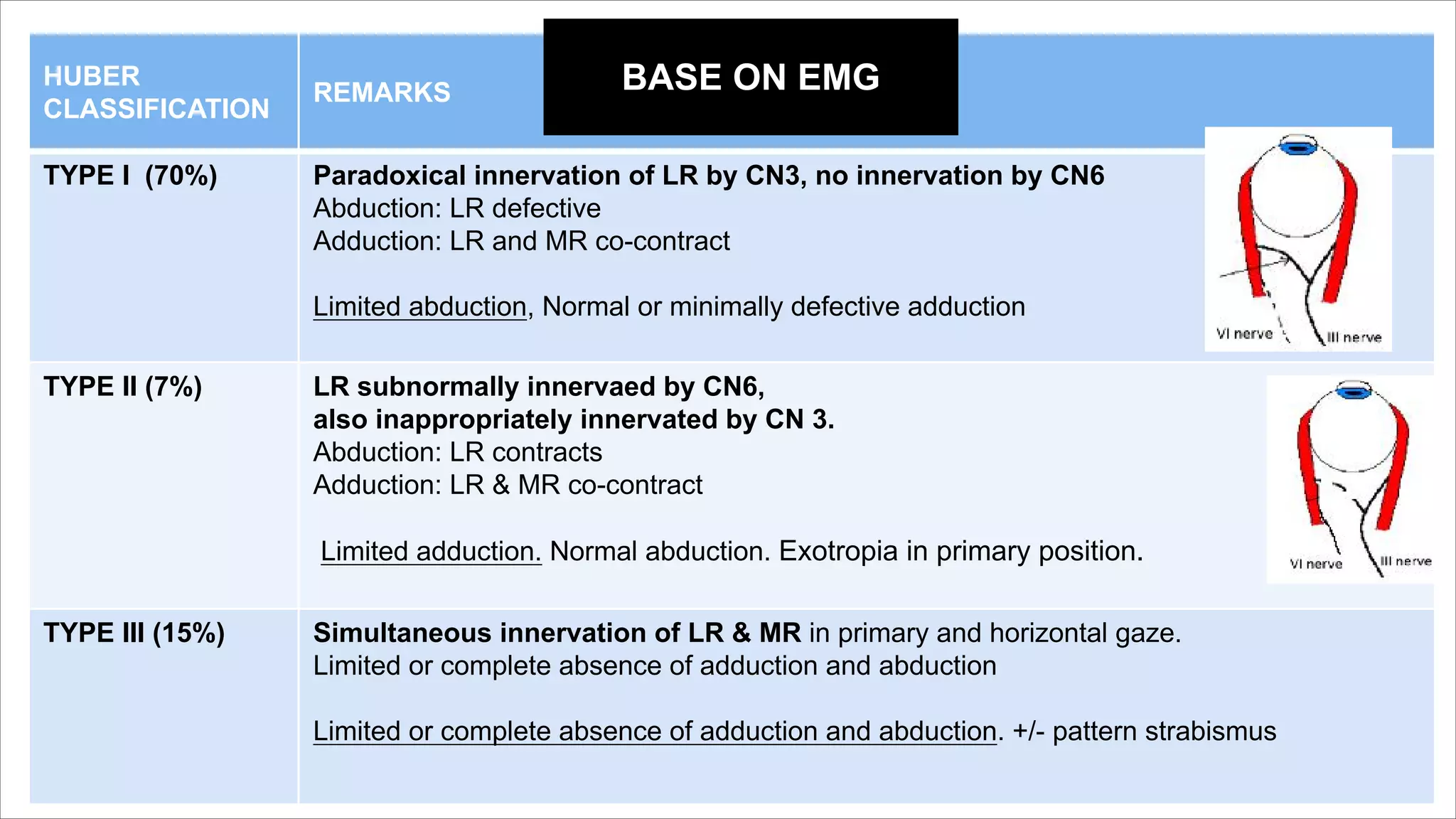
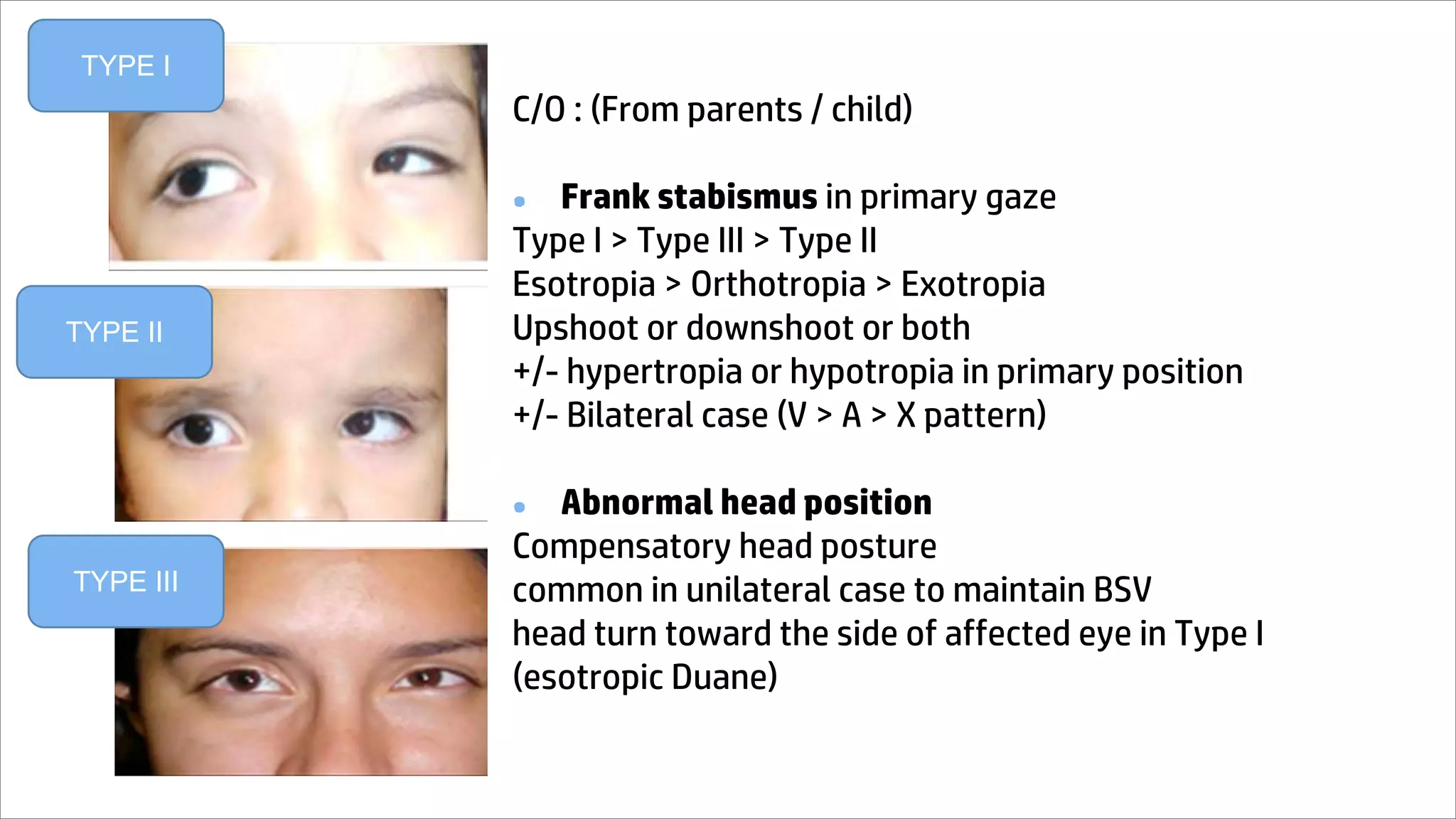
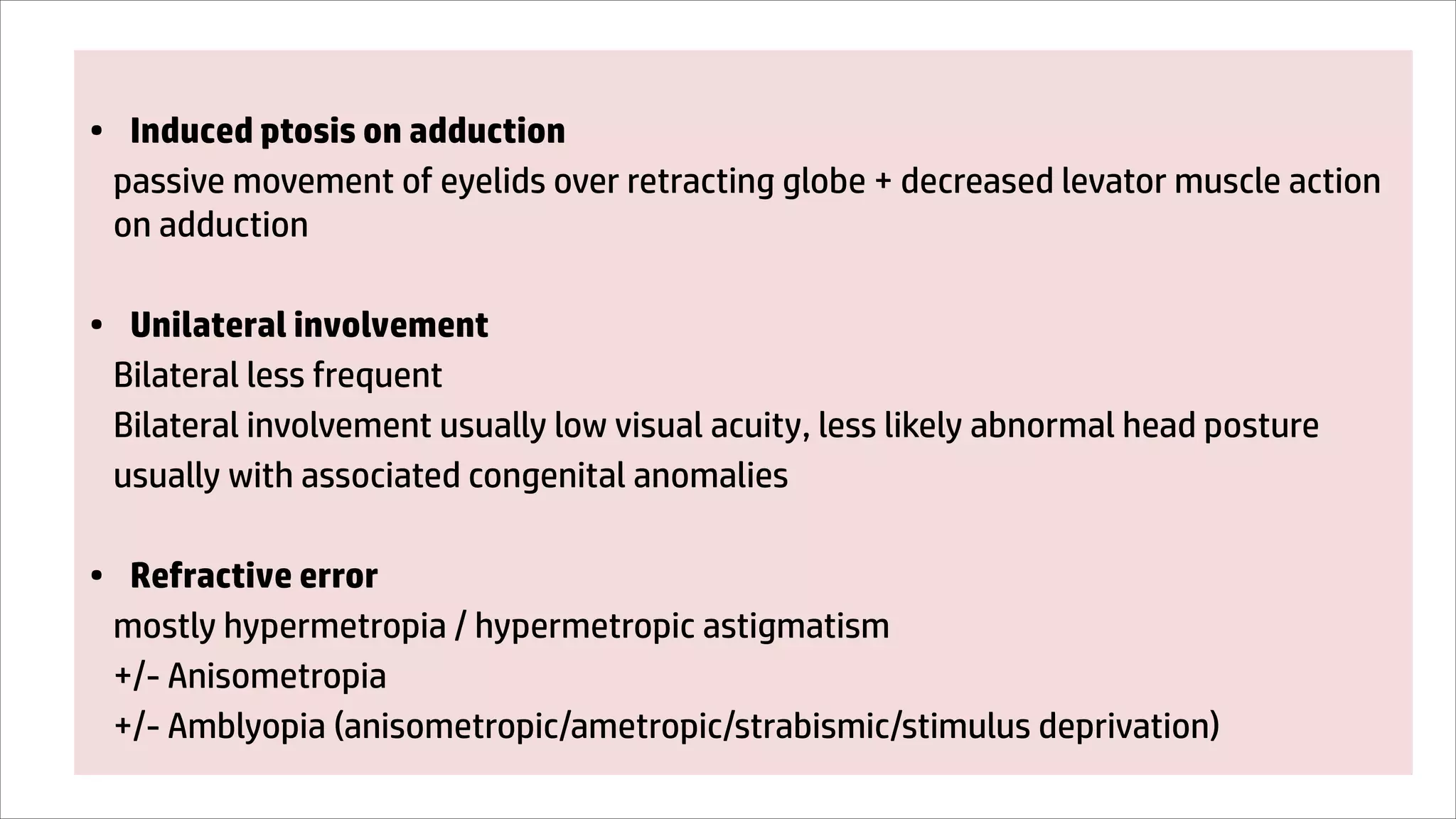
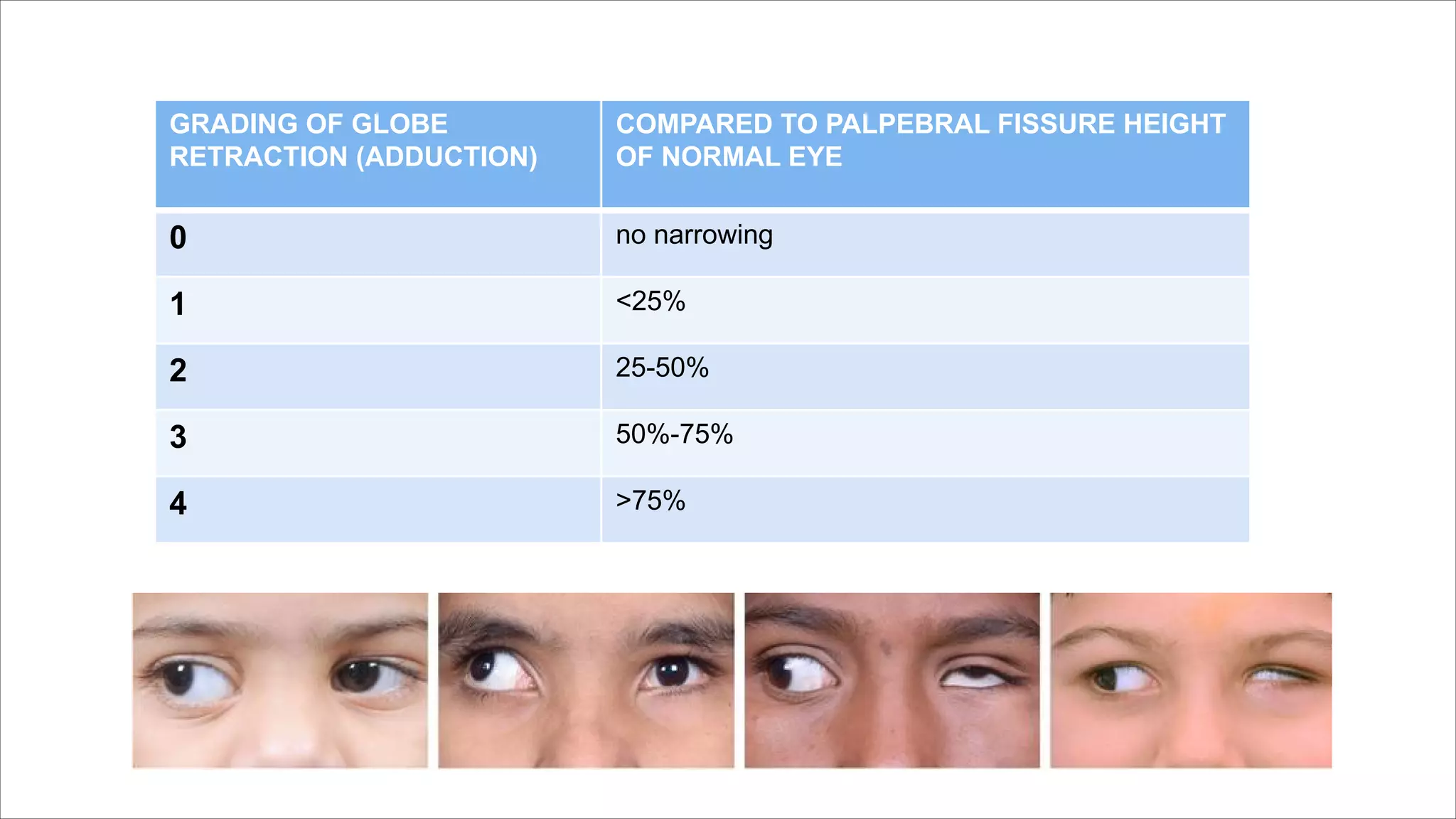
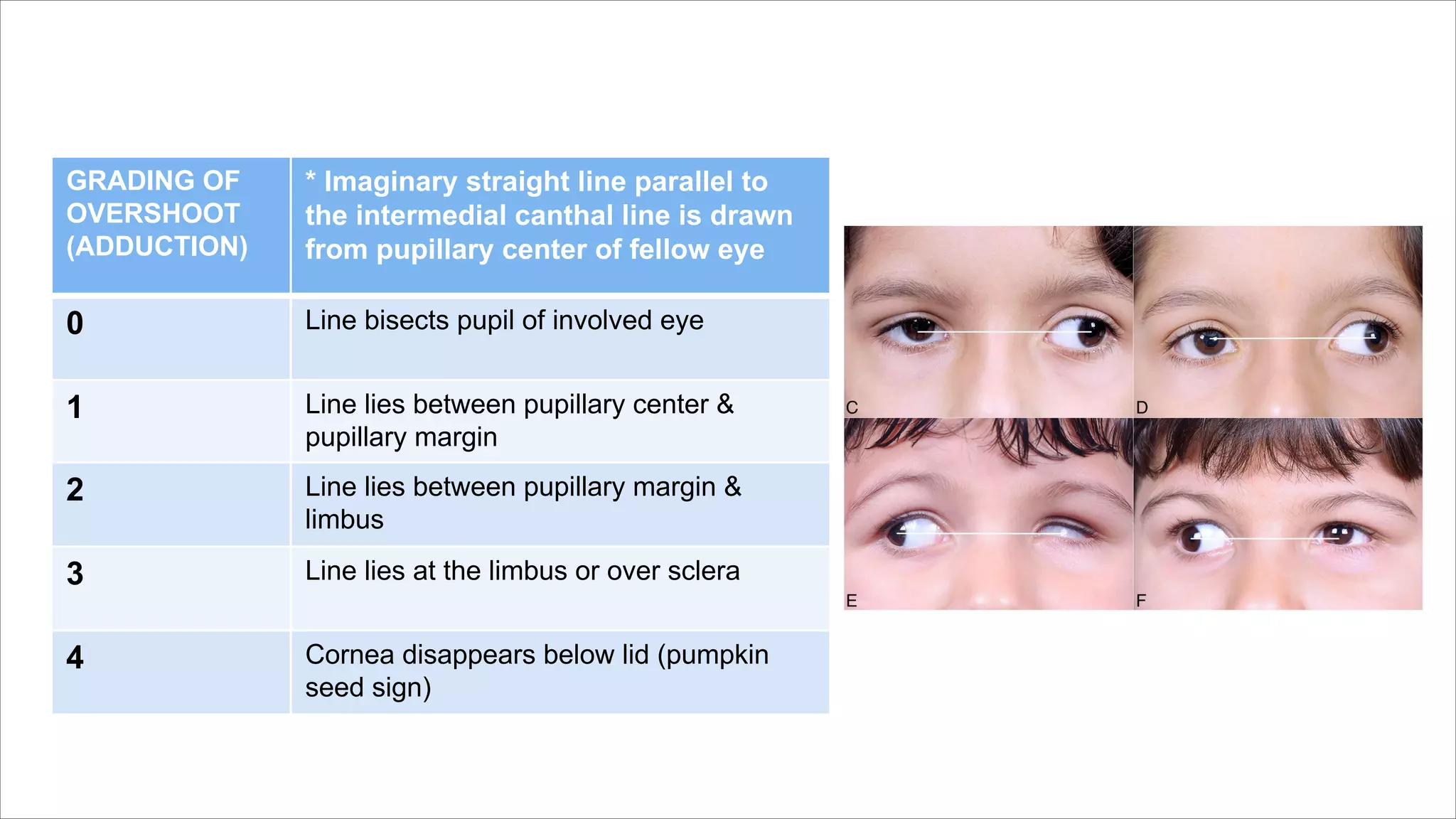
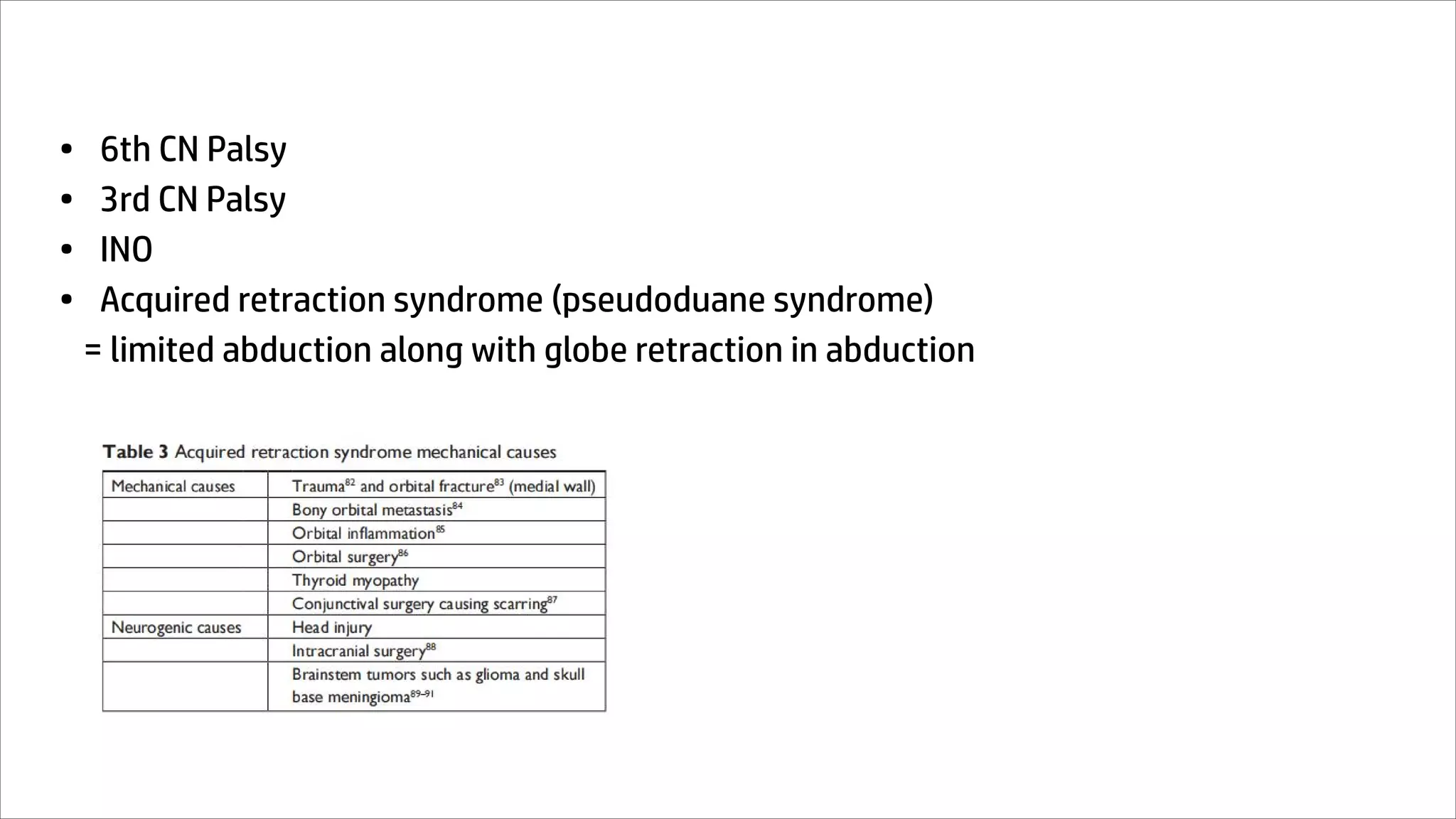
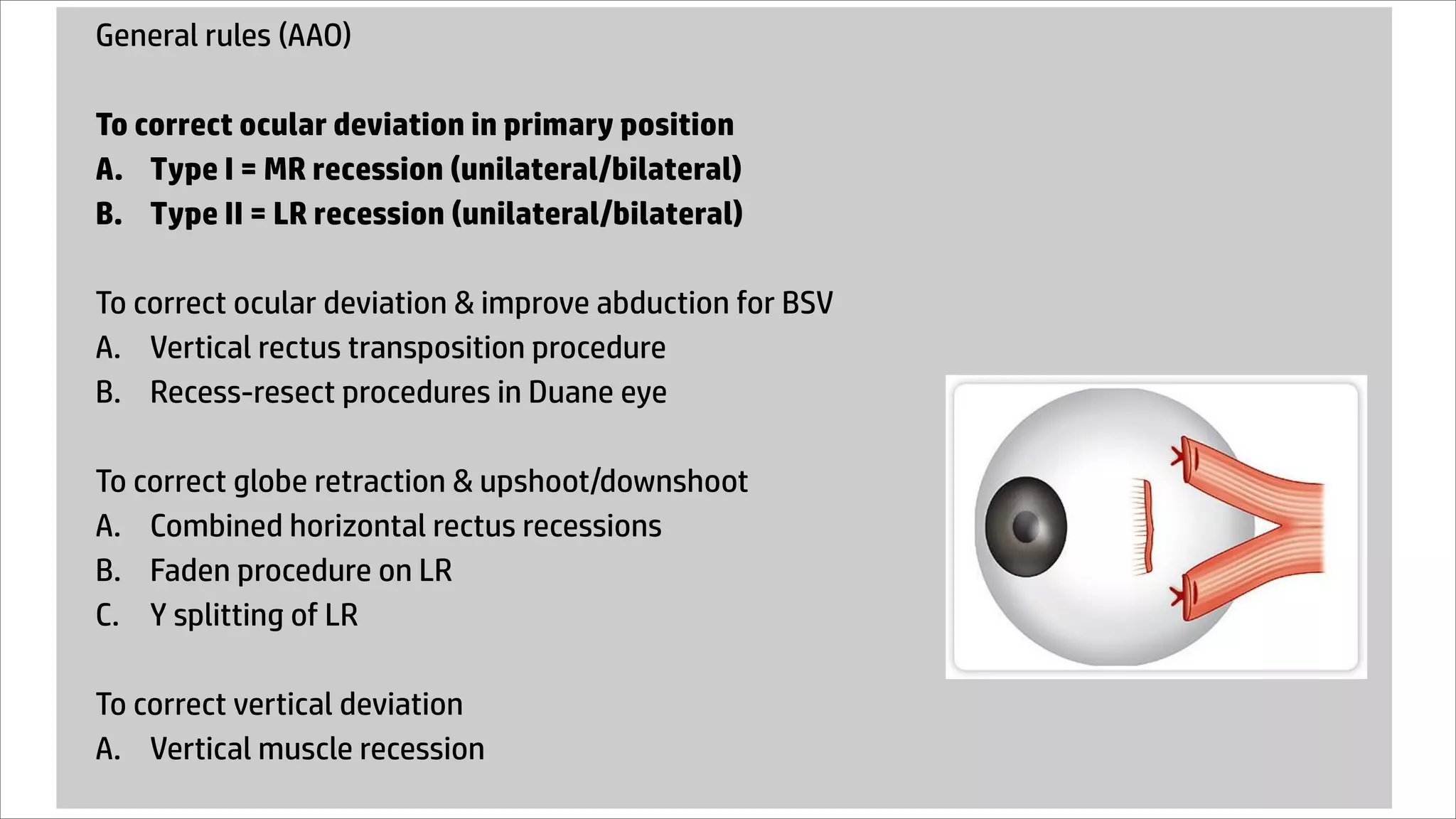
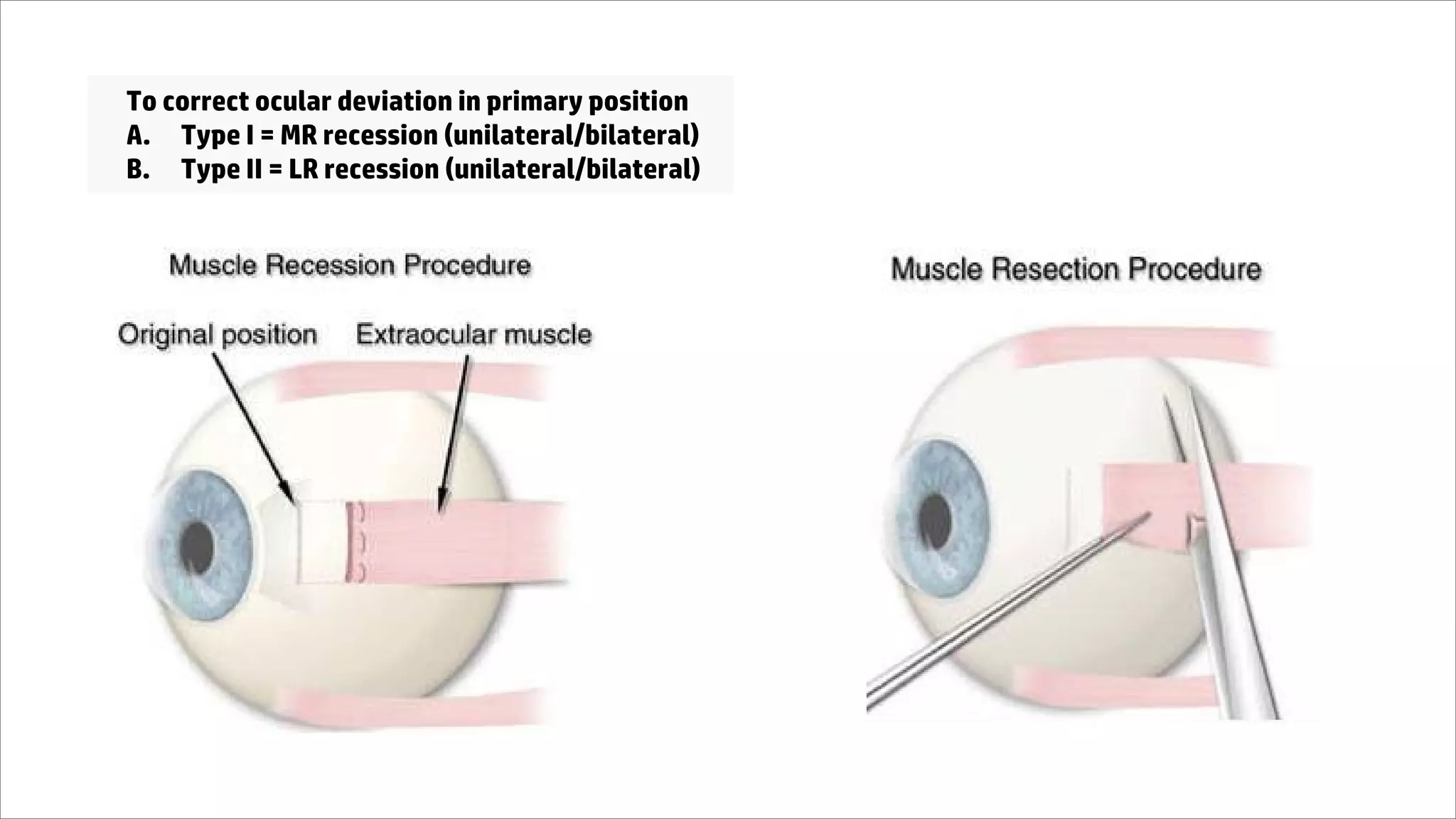
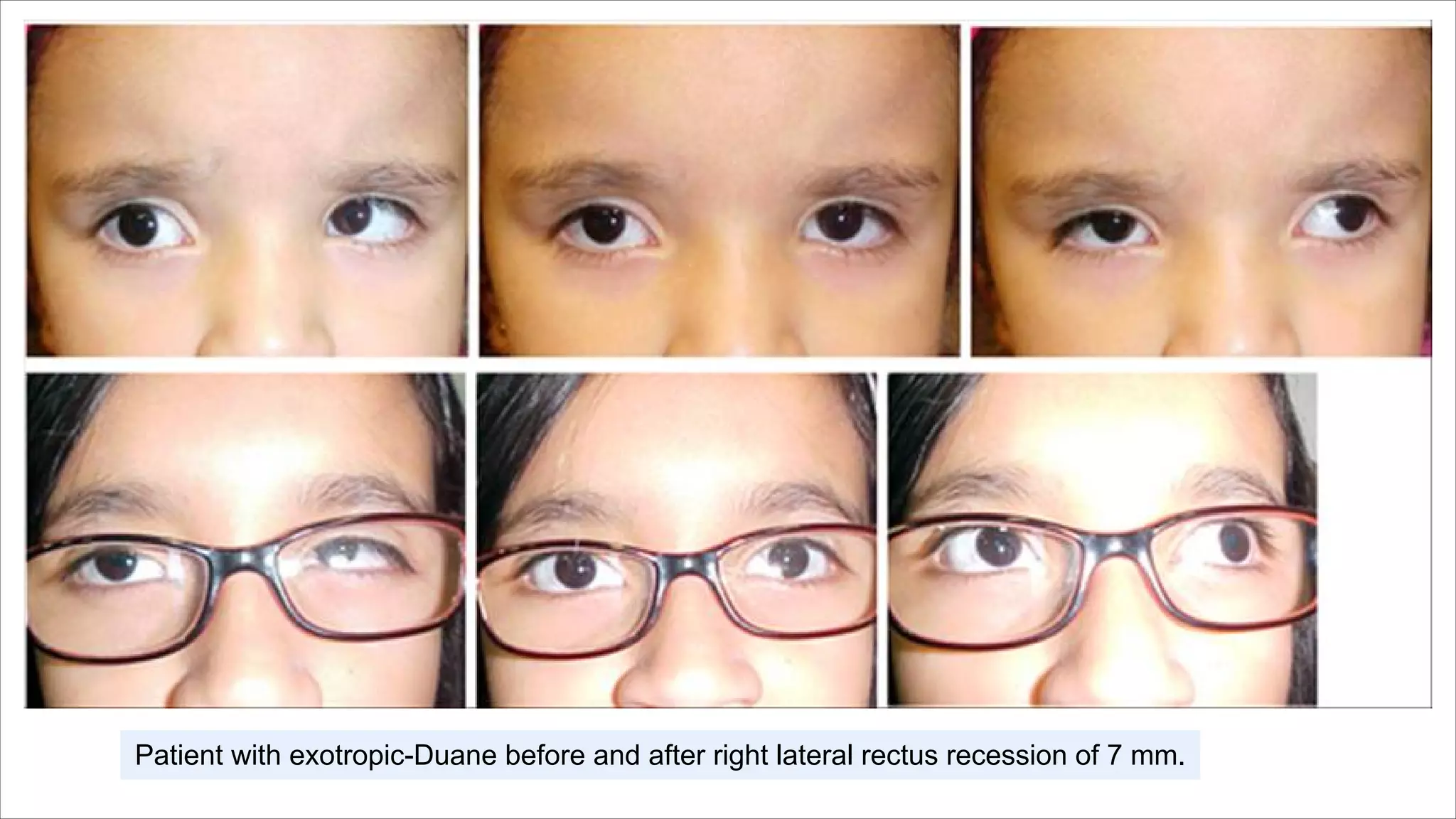
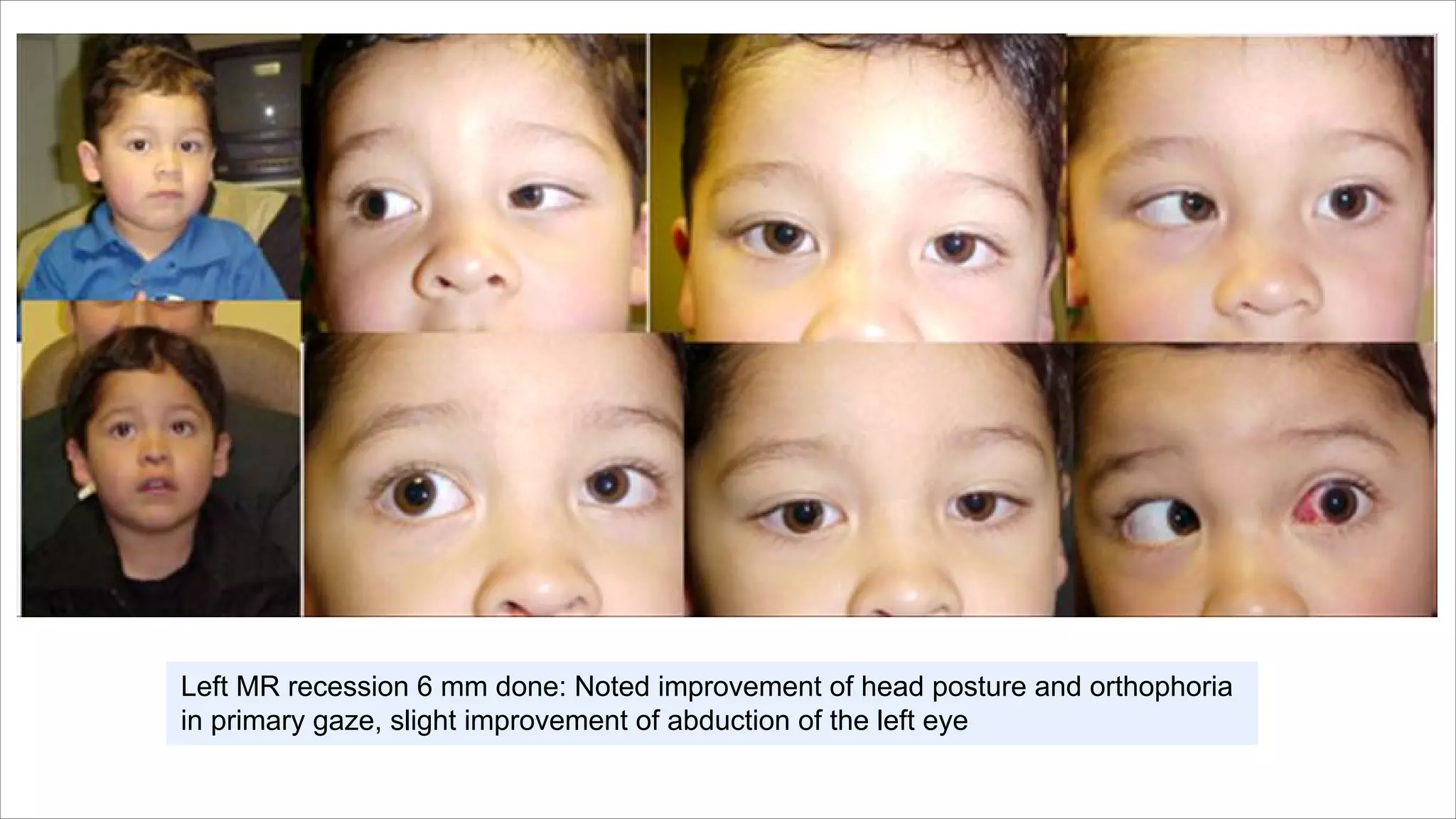
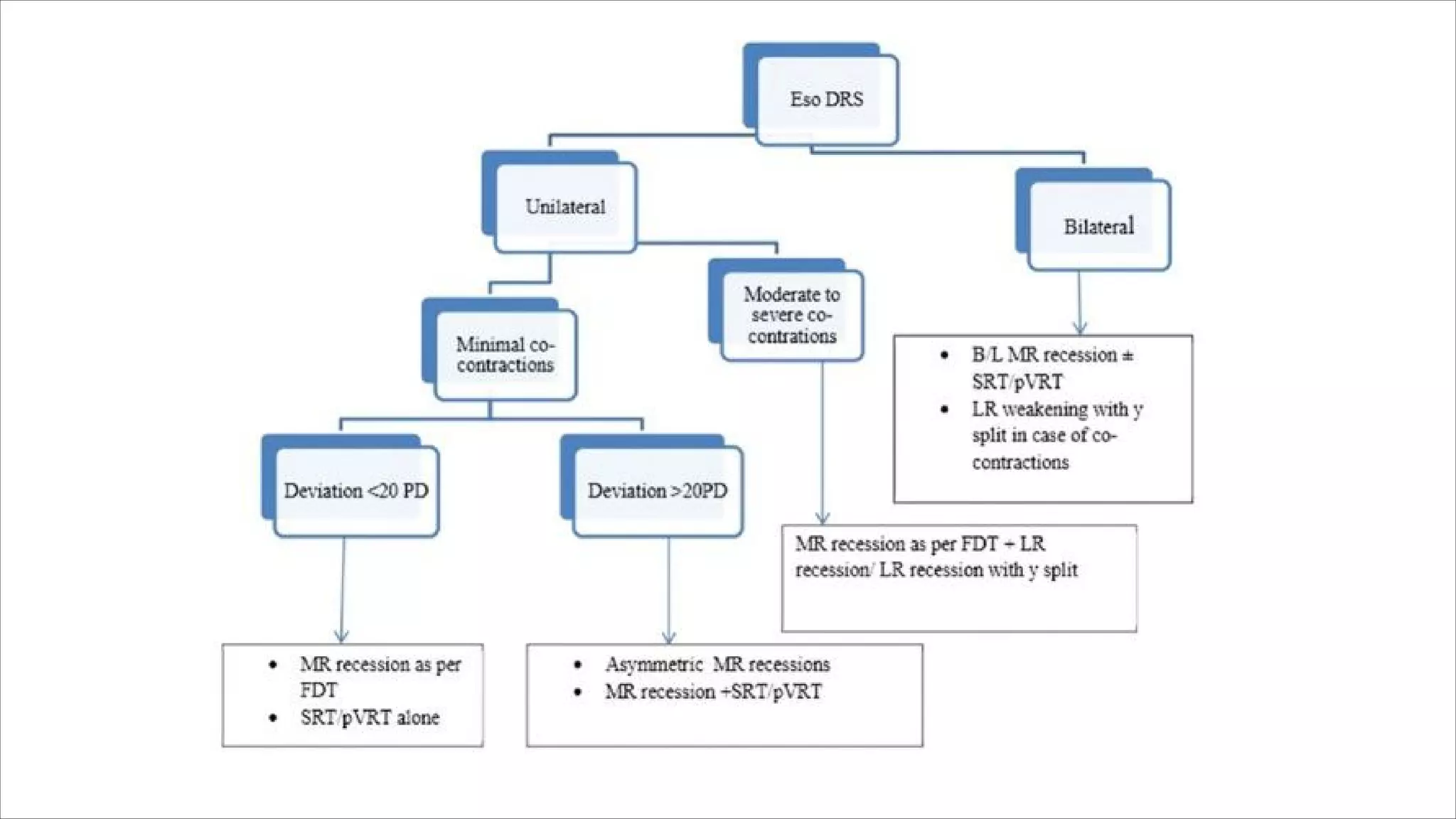
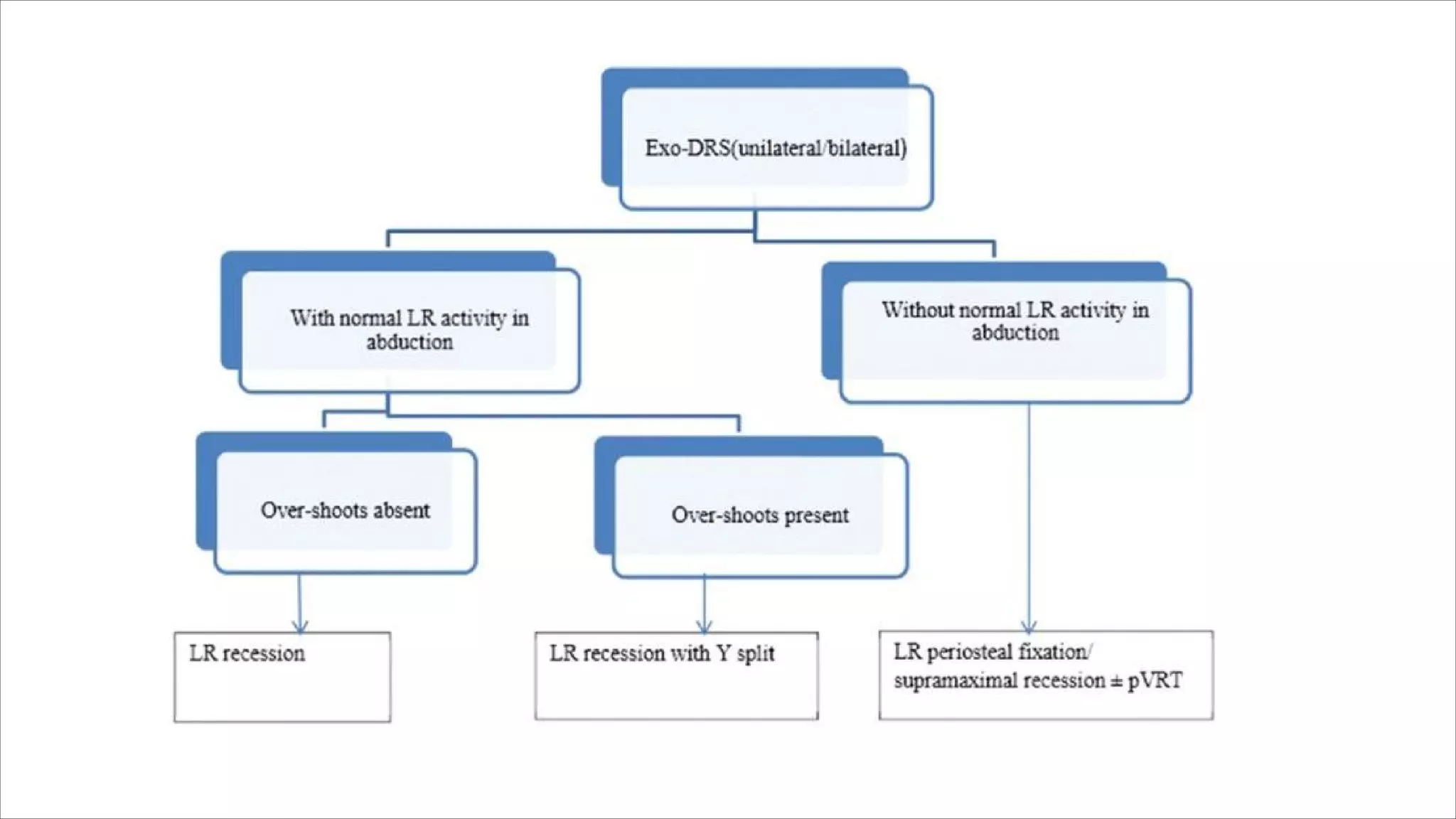
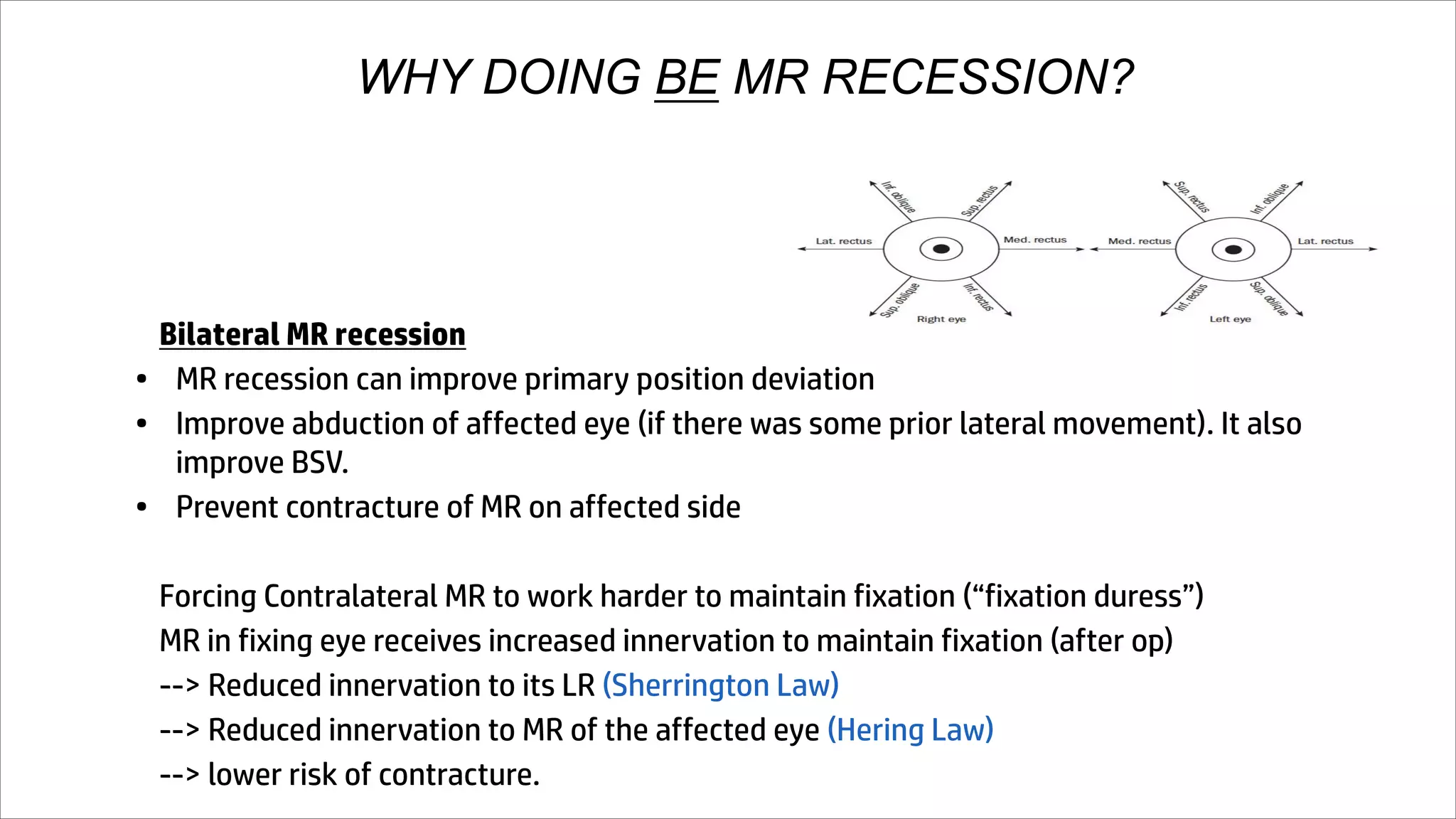
Duane Retraction Syndrome (DRS) is a congenital strabismus characterized by co-contraction of lateral (LR) and medial rectus (MR) muscles due to abnormal innervation, leading to limited eye movement and globe retraction. The condition can be classified into three types based on the degree of eye movement limitation and typically presents with associated conditions like amblyopia and abnormal head posture. Management may include conservative approaches like correction of refractive error and surgical interventions to improve eye alignment and function.