This document discusses the management of congenital and childhood cataracts from an optometrist's perspective, emphasizing the importance of early diagnosis, timely referral, and multidisciplinary collaboration for optimal outcomes. It includes a case presentation of a pediatric patient with congenital cataracts and outlines key challenges and surgical considerations, including the timing of surgery and refractive correction post-operation. Recommendations for managing visual impairments post-surgery, such as the use of corrective lenses or contact lenses, and the importance of amblyopia treatment strategies, are also highlighted.






































![IOL power calculation
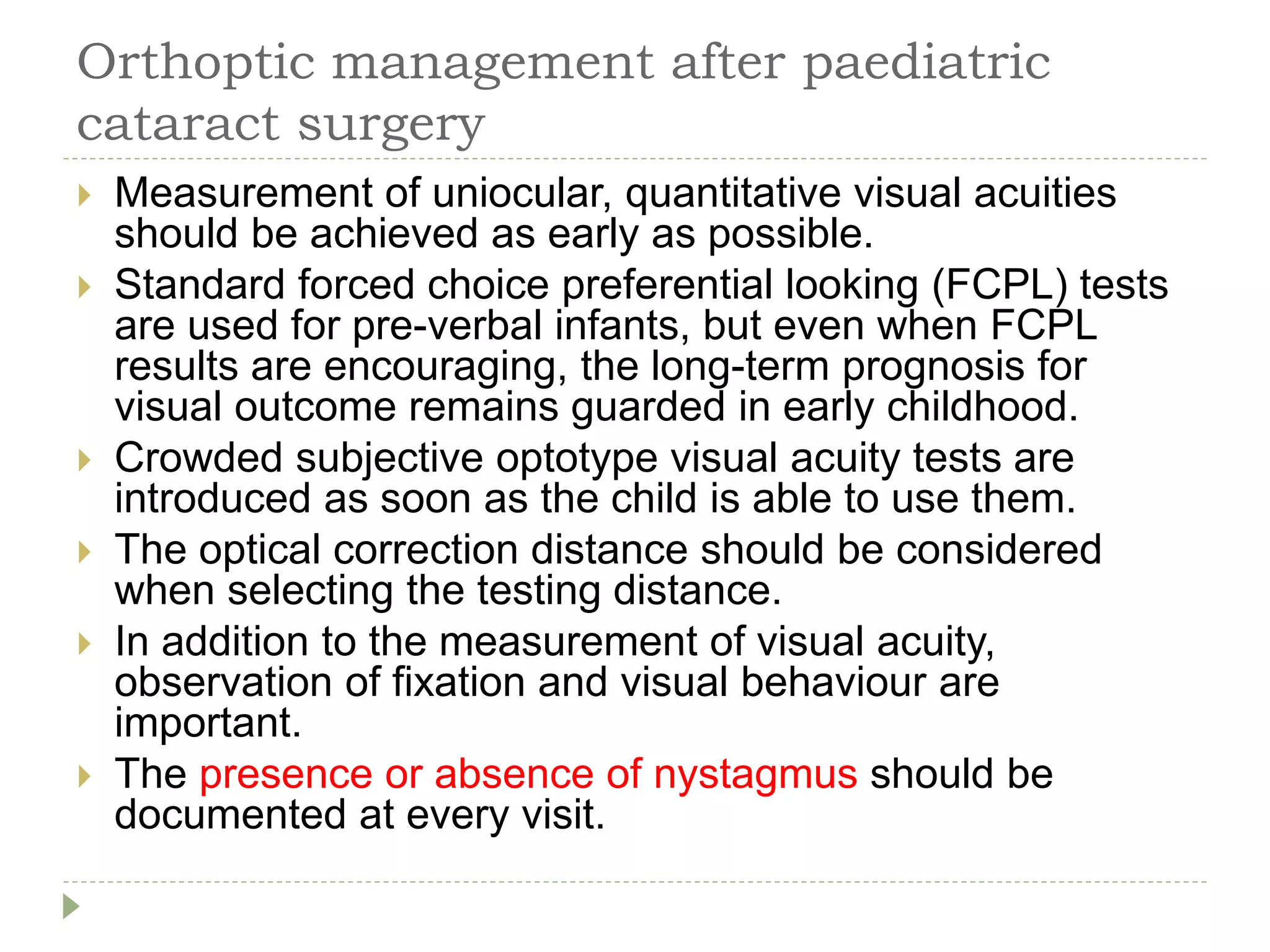
SRK II formula has been recommended [123] but
SRK/T and Holladay II formulae showed least
predictive error in a series of 117 eyes that included
eyes <20 mm axial length.
Thirty-one children with secondary IOL under 3.6
years were found to have the least median absolute
error with SRK II, SRK/T and Holladay I (1.23–
1.30D).
IOL master was deemed more accurate than contact
biometry method under general anaesthetic
(1.80 ± 1.40D vs. 2.43 ± 1.83D; p = 0.01).
The authors usually use the SRK-T formula and a
combination of SRK-T and Hoffer Q for short eyes.](https://image.slidesharecdn.com/cataractmanagementinchildrenfromoptometristperspective-210208081744/75/Cataract-management-in-children-from-optometrist-perspective-40-2048.jpg)



