Here are the answers to the MCQs:
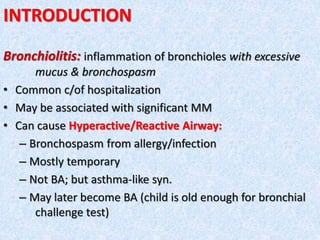
1. RSV is the commonest c/of bronchiolitis - True
2. ABT is usually required in B - False
3. Most B are later associated with BA - True
4. In EBF babies B is rare - True
5. Anticholingergic nebulization is beneficial in B - False
6. B is usually a killer D - False
7. SARS/MERS is caused by RSV - False
8. Antiviral Rx is beneficial in all B cases - False