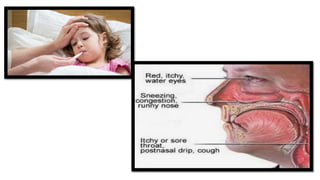
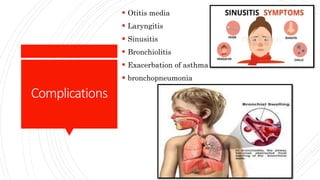
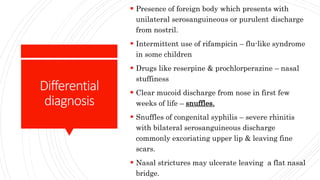
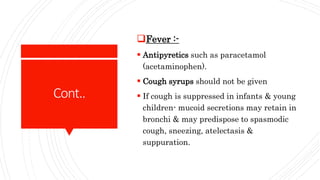
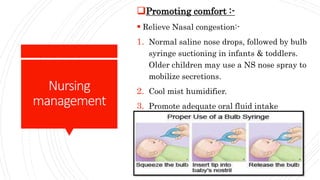
The document discusses the common cold or nasopharyngitis in children. It is a frequent illness in childhood caused by viral infections of the upper respiratory tract. Clinical manifestations include fever, nasal congestion, sore throat, cough and runny nose. Diagnosis is made based on symptoms and physical examination. Treatment is generally supportive with antipyretics, nasal decongestants, and increased fluid intake. Complications may include ear infections, sinusitis or lower respiratory infections. Nursing care focuses on relieving symptoms, adequate rest and fluid intake, with a goal of promoting comfort and effective airway clearance. Prevention involves frequent hand washing and avoiding close contact with those exhibiting cold symptoms.