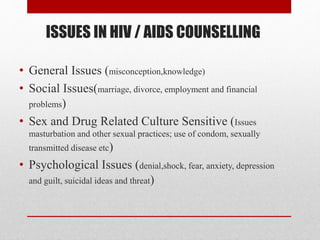
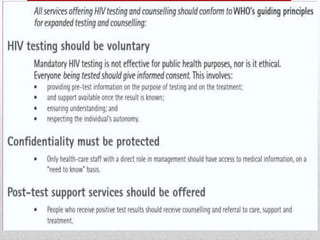
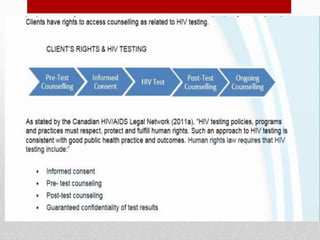
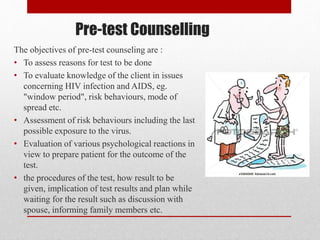
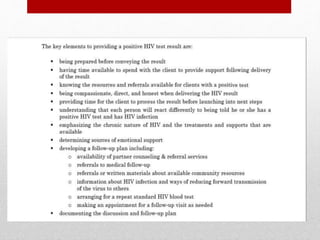
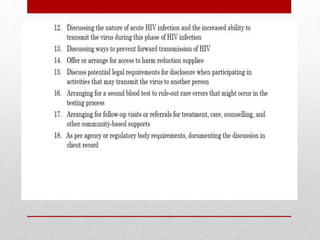
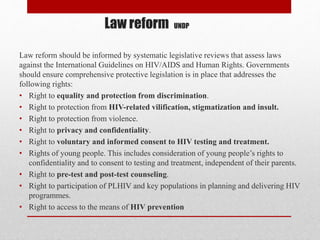
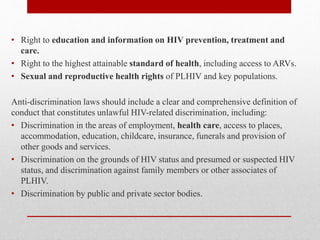
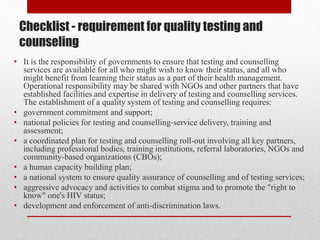
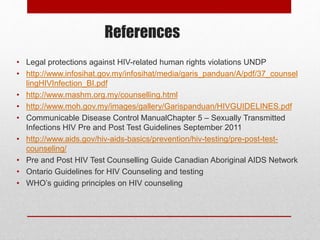
HIV/AIDS counseling involves a trained counselor helping clients address issues related to HIV, including prevention and psychosocial support. Key objectives include promoting healthy behaviors, providing accurate information, and ensuring informed consent, especially during pre- and post-test counseling stages. The document emphasizes the need for confidentiality, understanding client fears, and adhering to legal protections for those affected by HIV/AIDS.