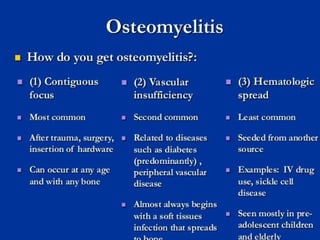
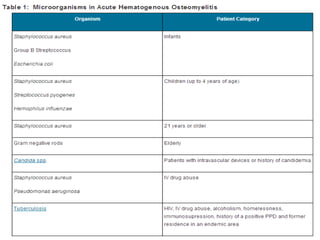
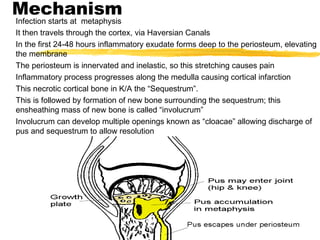
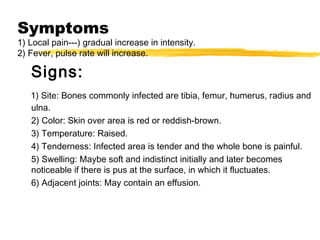
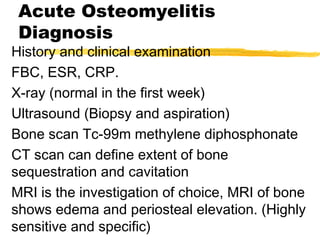
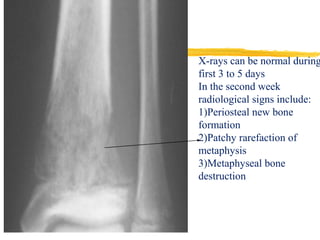
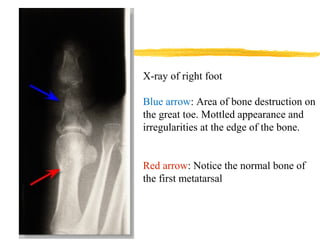
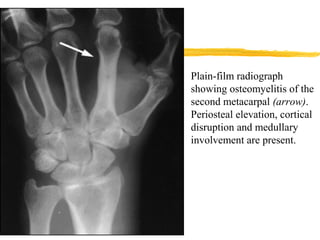
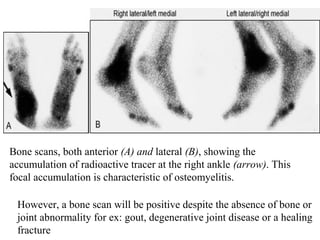
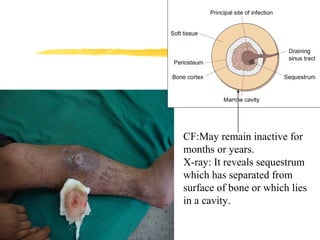
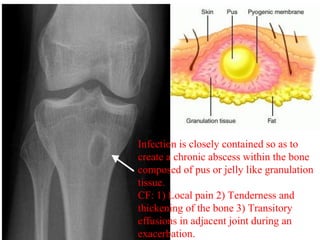
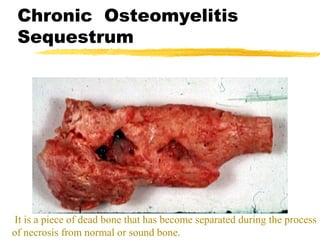
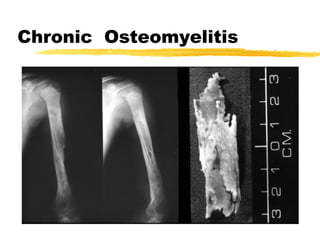
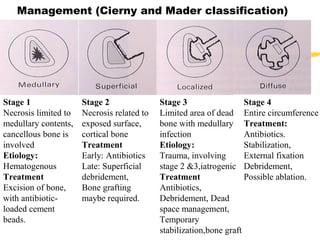
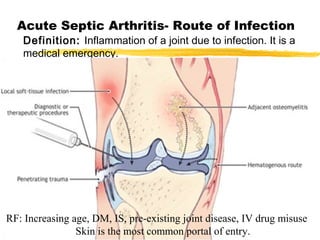
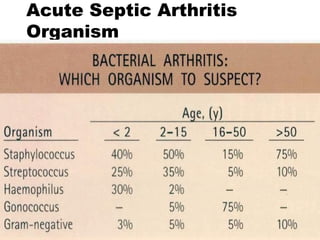
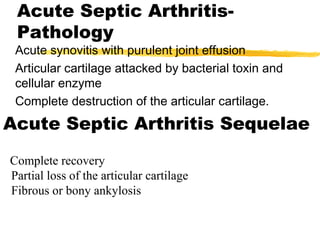
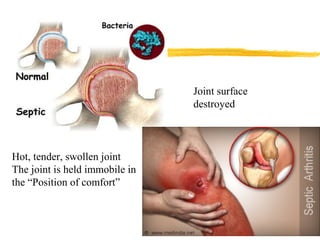
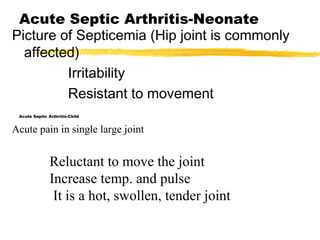
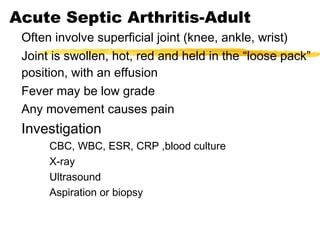
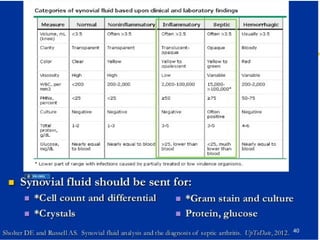
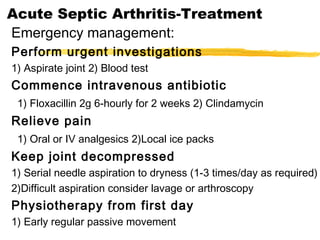
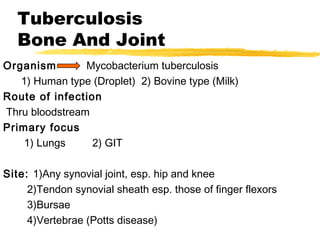
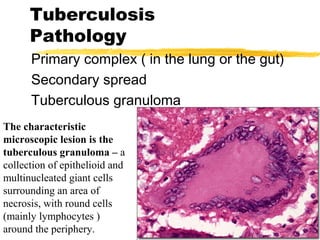
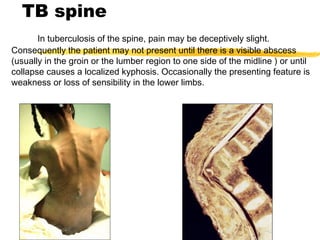
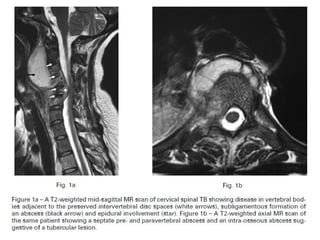
The document discusses infection of bone and joint, including osteomyelitis, septic arthritis, and tuberculosis. It provides details on the mechanisms, symptoms, investigations, and treatments for acute and chronic osteomyelitis. It describes how septic arthritis can infect joints via the bloodstream or skin. Tuberculosis is caused by Mycobacterium tuberculosis and can infect synovial joints, tendon sheaths, and vertebrae, leading to granuloma formation, joint destruction, and abscesses. Treatment involves chemotherapy with rifampicin and isoniazid.