This document provides information on congenital pseudarthrosis of the tibia (CPT), including:
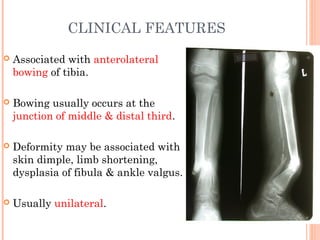
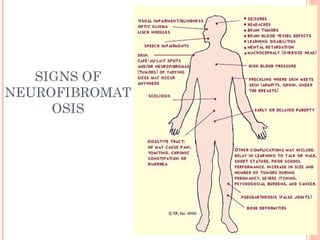
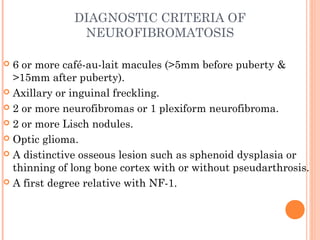
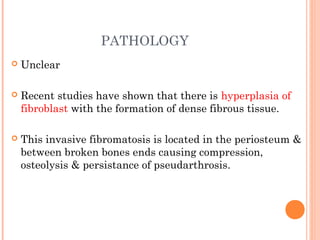
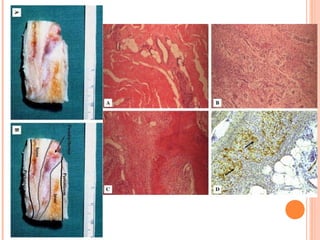
- CPT is a nonunion of the tibia that develops spontaneously in early life and is associated with bowing of the tibia. It occurs more commonly in patients with neurofibromatosis type 1.
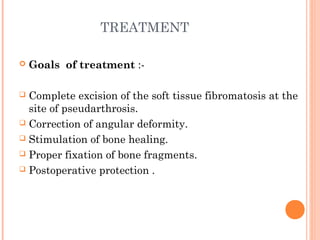
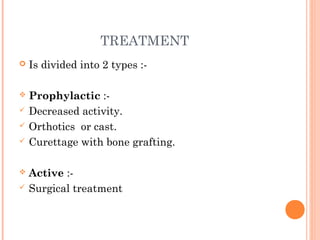
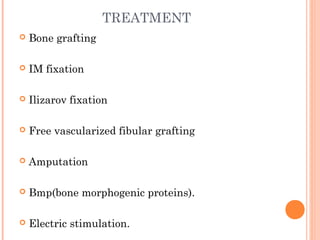
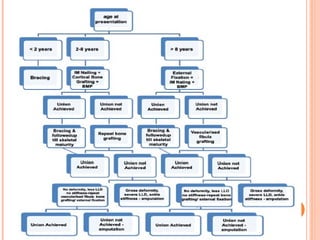
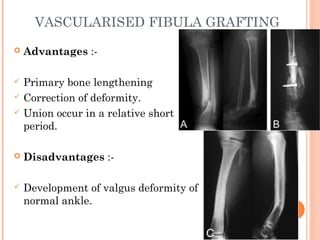
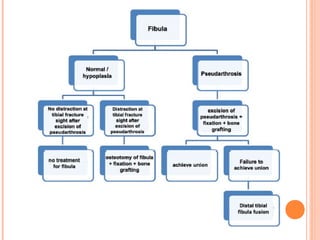
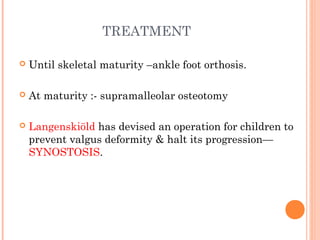
- Surgical treatment aims to completely excise fibrous tissue, correct deformity, stimulate bone healing, and properly fix bone fragments. Options include bone grafting, internal fixation, Ilizarov fixation, vascularized fibular grafting, and amputation in severe cases.
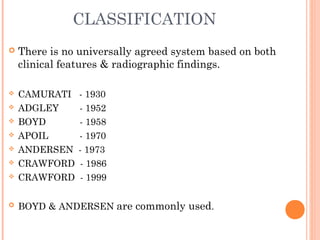
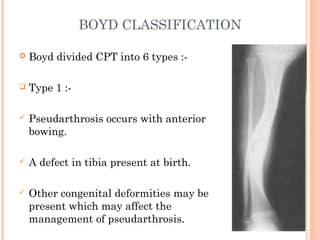
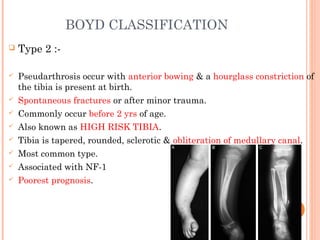
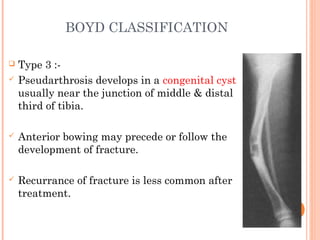
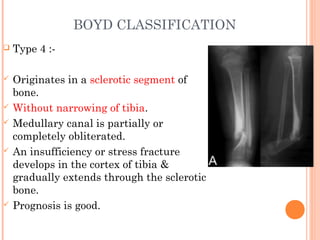
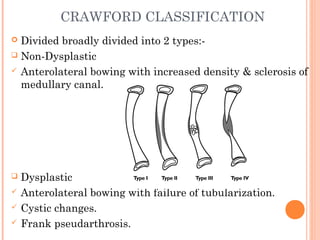
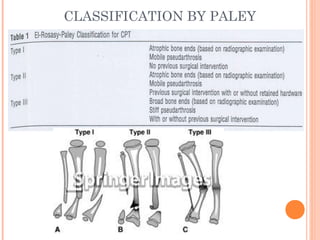
- Classification systems divide CPT into types based on clinical features and radiographic findings to help determine prognosis and guide treatment