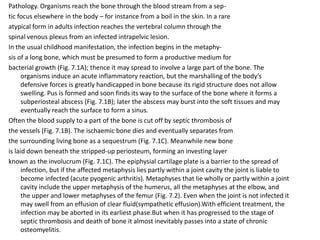
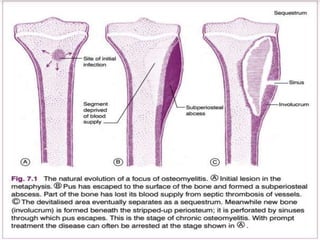
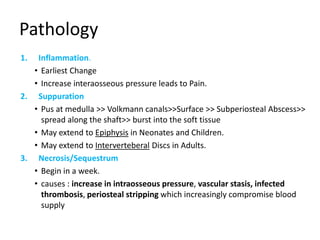
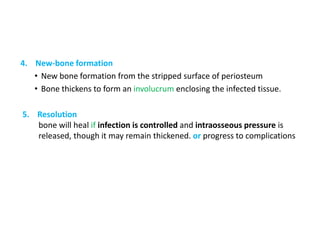
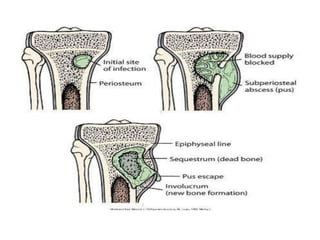
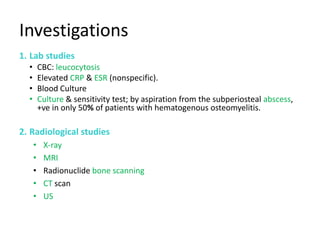
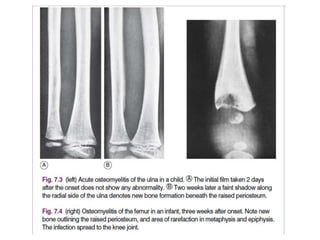
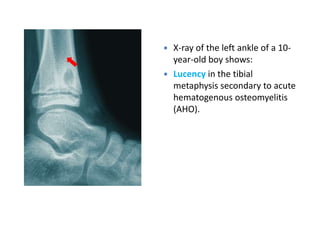
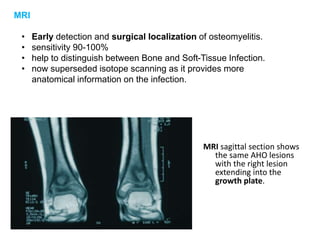
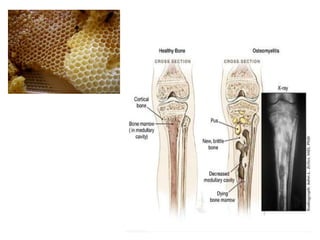
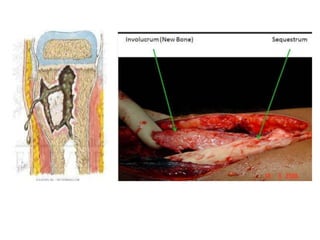
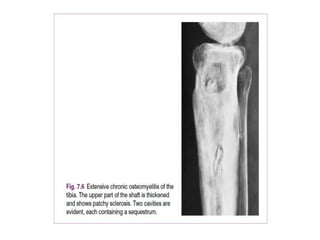
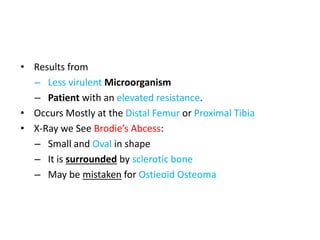
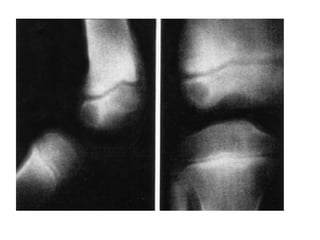
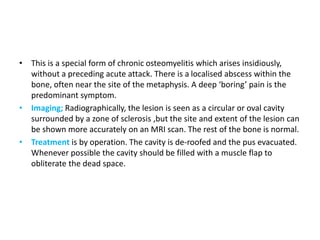
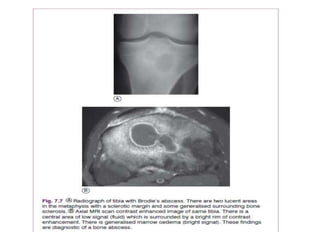
Osteomyelitis is an infection of the bone caused by microorganisms, typically reaching bones via the bloodstream or direct invasion. It is classified based on duration (acute, subacute, chronic) and commonly affects children in long bones while adults often have infections in the vertebrae. Diagnosis involves lab studies and imaging, with treatment requiring antibiotics and possibly surgical intervention, but chronic cases can complicate management and lead to ongoing health issues.