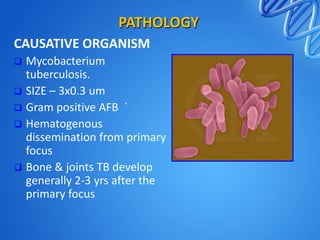
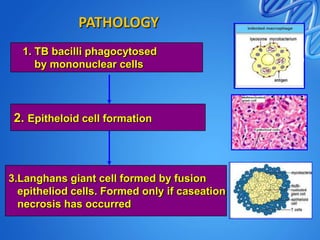
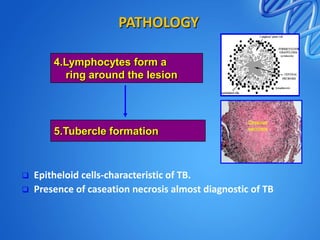
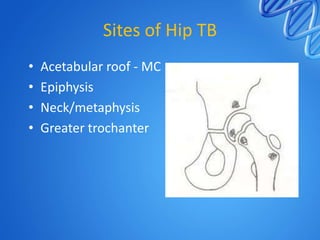
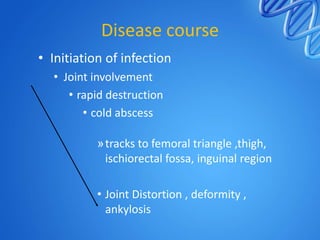
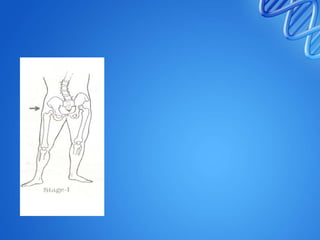
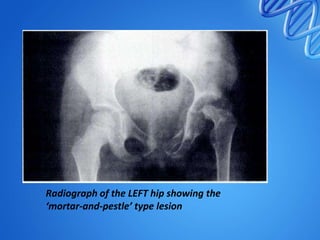
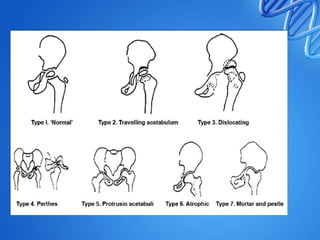
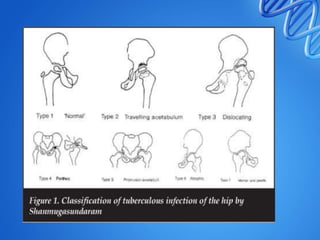
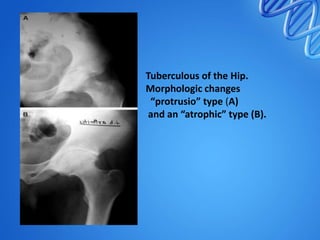
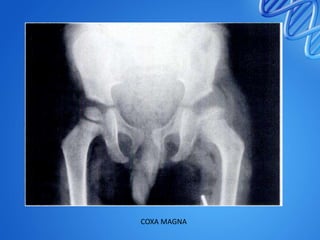
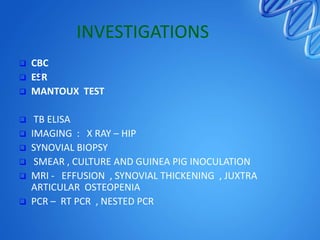
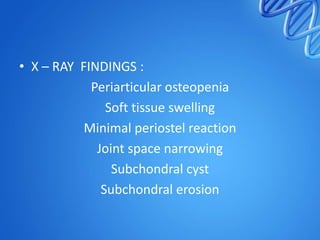
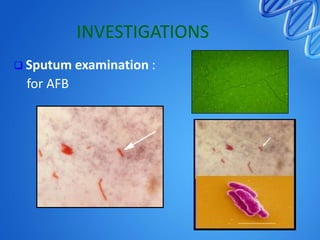
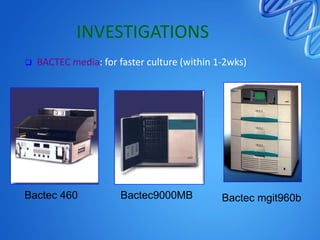
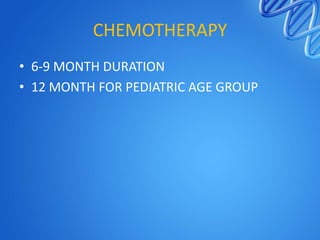
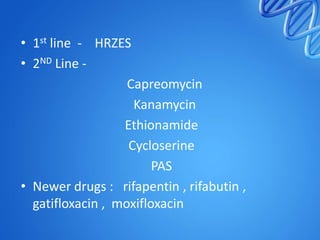
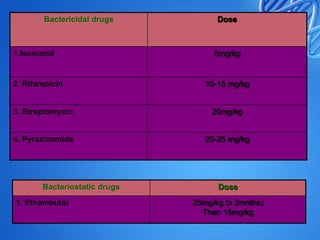
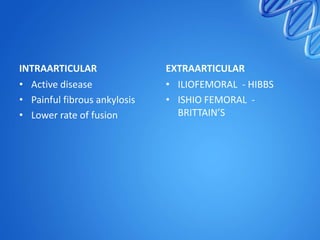
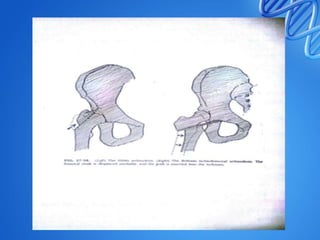
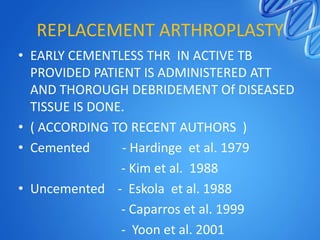
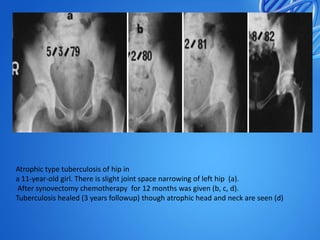
Tuberculosis of the hip is caused by Mycobacterium tuberculosis infection. It typically affects people aged 20-30 years old. The infection spreads hematogenously from a primary focus and causes destruction of bone and joints over several years. Clinical features include limping, decreased range of motion, and deformities in advanced cases. Imaging shows osteopenia, joint space narrowing, and bone erosion. Treatment involves chemotherapy for at least 6-9 months along with local measures like joint aspiration and traction. Surgery may be needed for debridement, arthrodesis, or arthroplasty in advanced cases.