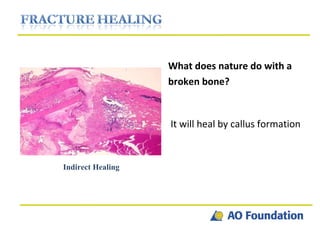
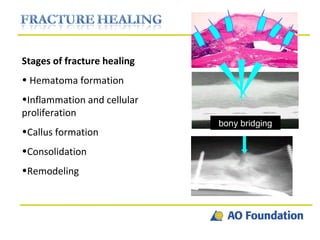
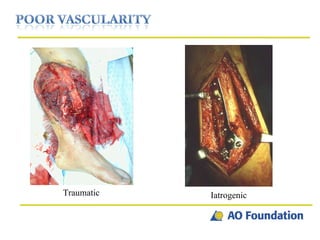
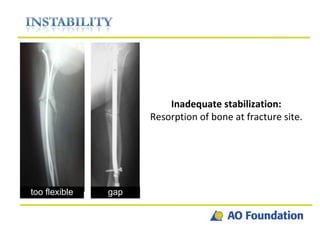
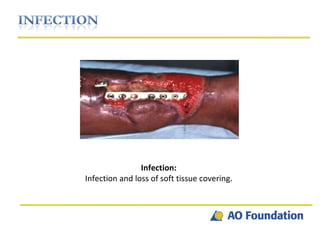
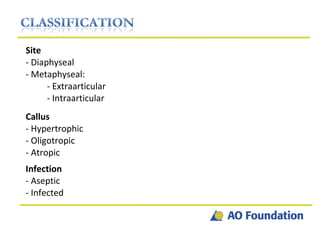
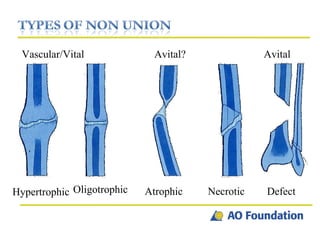
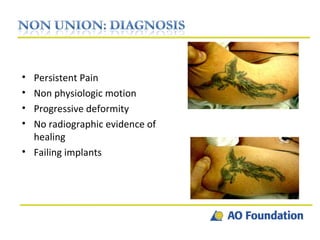
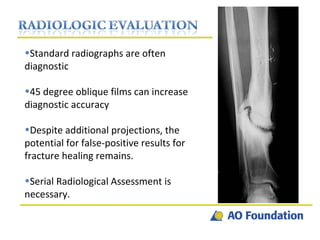
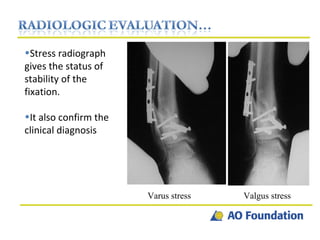
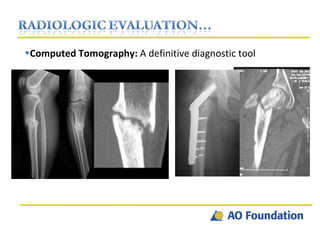
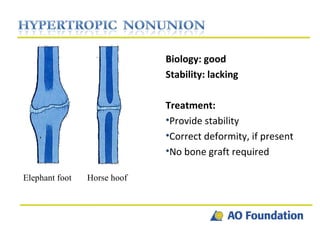
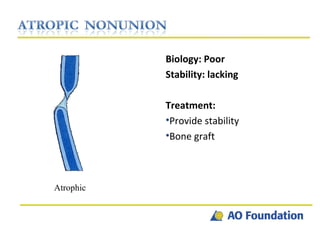
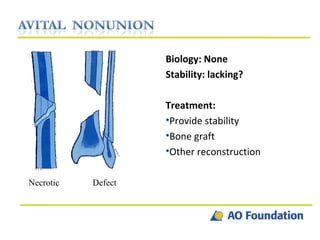
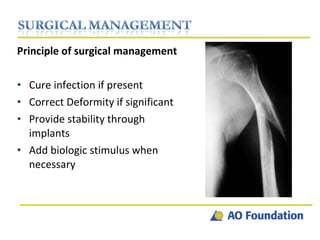
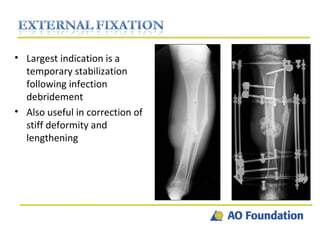
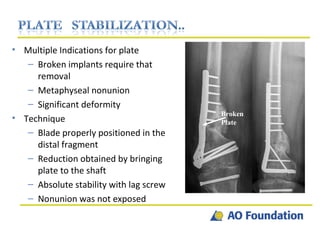
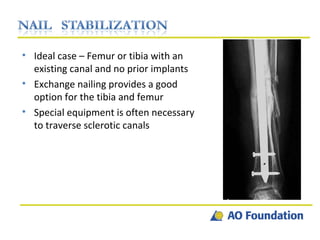
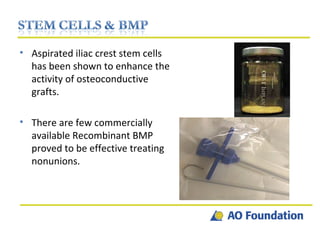
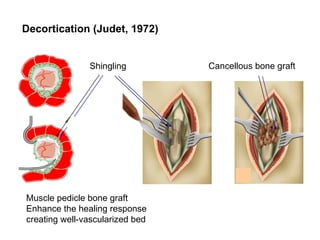
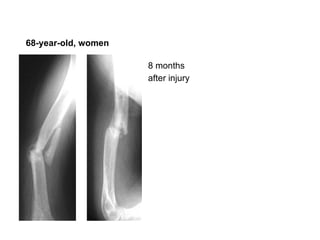
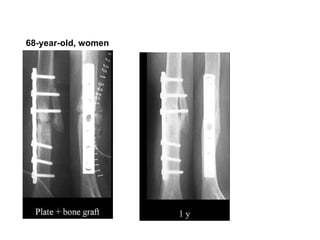
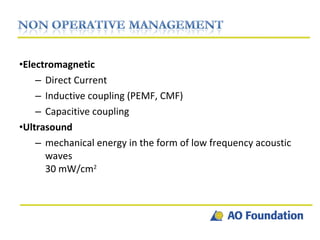
The document discusses non-union and delayed union in fractures, including definitions, causes, and treatment principles. It emphasizes the importance of stability, biological factors, and infection management in promoting fracture healing. Various surgical techniques and biological interventions are outlined for addressing different types of non-unions and enhancing healing outcomes.