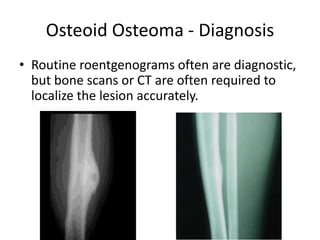
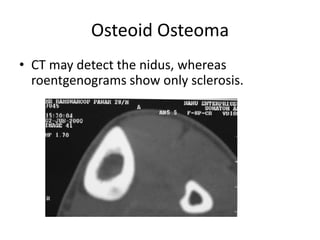
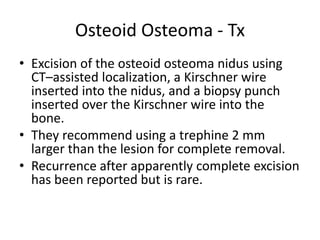
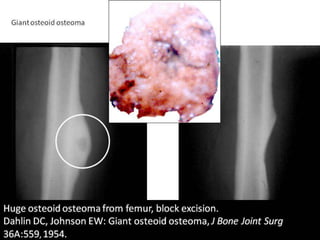
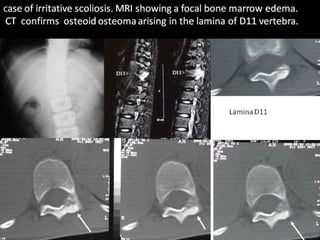
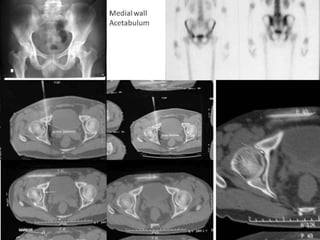
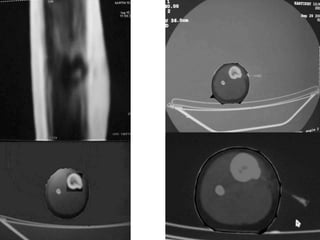
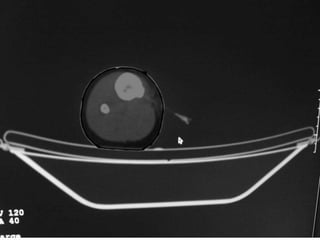
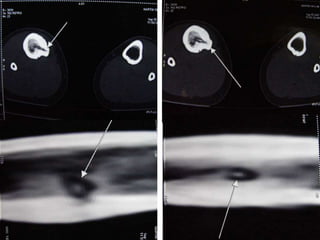
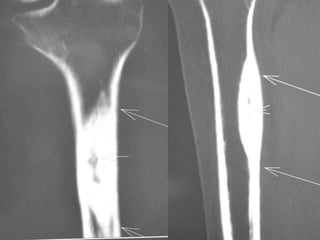
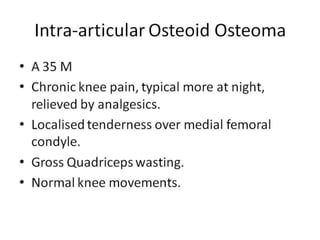
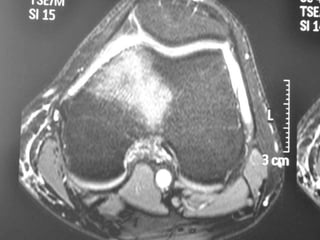
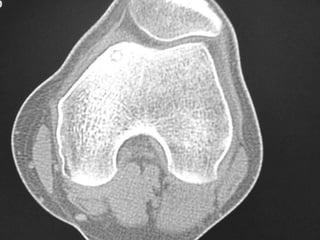
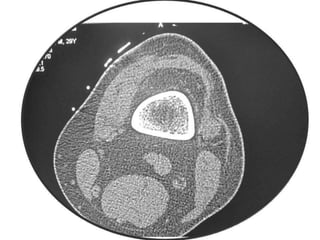
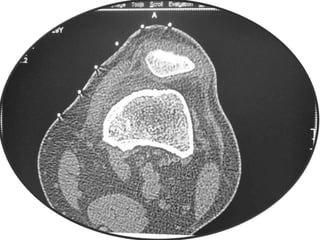
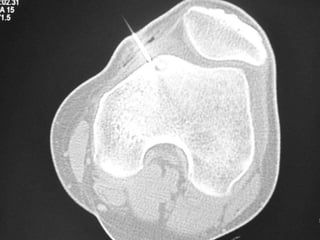
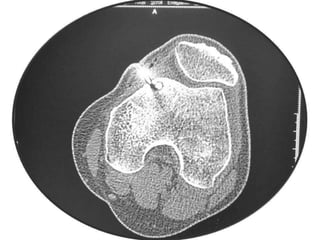
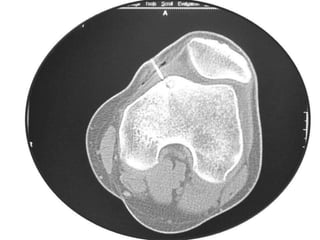
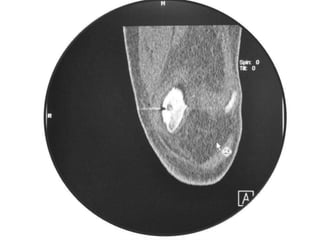
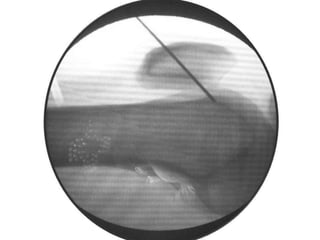
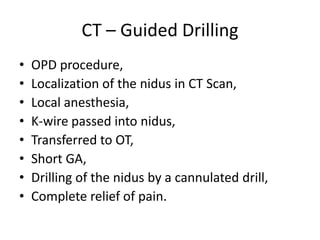
This document summarizes information about osteoid osteoma, a benign bone tumor. It describes the typical presentation as a painful lesion most common in younger males, often located in the femur or tibia. Diagnosis typically involves x-ray, CT scan or bone scan to locate the lesion. While traditionally treated with open surgical excision, minimally invasive techniques like CT-guided percutaneous excision have high success rates with less morbidity.