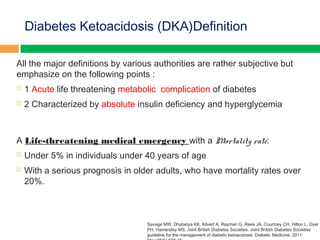
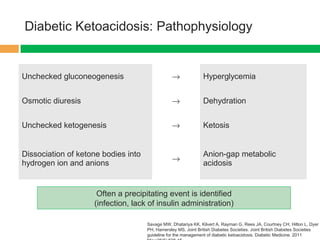
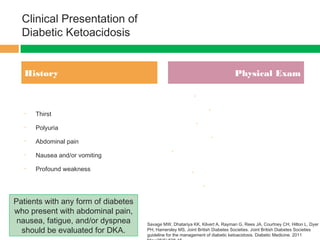
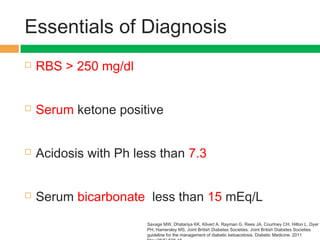
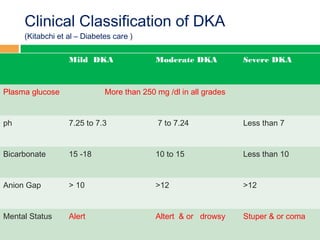
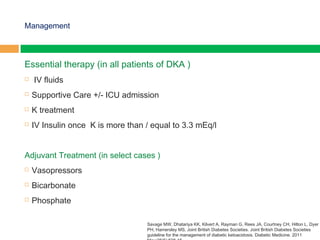
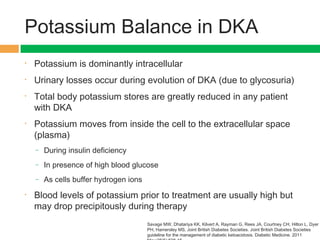
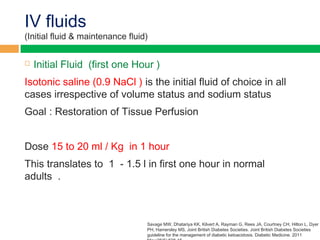
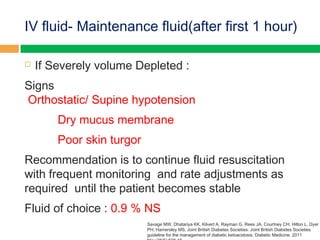
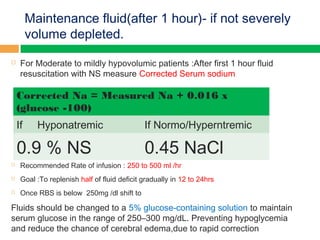
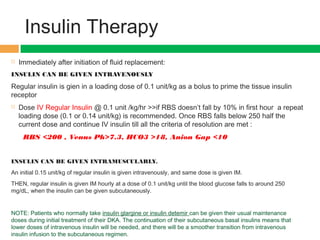
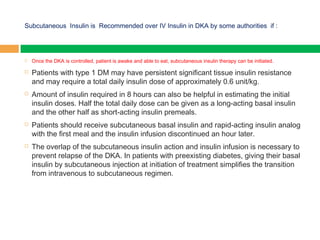
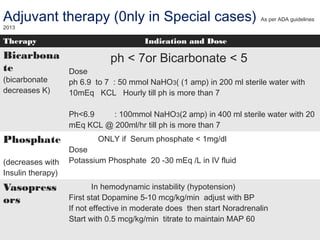
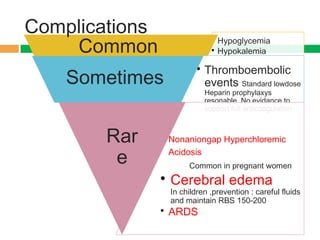
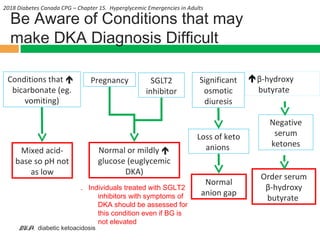
Diabetic ketoacidosis (DKA) is a life-threatening complication of diabetes caused by absolute insulin deficiency and hyperglycemia. It is characterized by dehydration, ketosis, and metabolic acidosis. Symptoms include nausea, vomiting, and abdominal pain. If untreated, DKA can lead to stupor and coma. Treatment involves intravenous fluids, electrolyte replacement, insulin therapy, and identifying and treating any precipitating causes. Careful monitoring of glucose, electrolytes, pH, and fluid balance is needed to safely resolve the condition. Complications can include hypoglycemia, hypokalemia, and in rare cases, cerebral edema or acute respiratory distress syndrome.